What is Allergy?
Links to online patient groups
Immunotherapy for Bee and Wasp Venom Allergy Patient Information
What is immunotherapy?
Immunotherapy, also called desensitisation, is the only treatment that can reduce the risk of anaphylaxis in individuals who are allergic to bees or wasps. The treatment involves administering small amounts of the protein which the person is allergic to (which is called an allergen) so that the body can slowly “get used” to it. This will reduce the chances of the person having a severe reaction if they are stung by the bee or wasp again.
This treatment is very effective, providing >95% protection against serious wasp venom reactions and about 90% protection against serious reactions to a bee sting.
What your treatment involves
Immunotherapy treatment is given as injections just beneath the skin (subcutaneously).
Initially, you will receive slowly increasing doses of the venom allergen on a weekly basis for 12 weeks. We will then give a maintenance dose every 4 to 6 weeks for up to 2 years and then 6-8 weekly for the third (final) year.
The injections will be administered in the outpatient department under medical supervision. You will be asked to stay for one hour after your injection in case of any reactions. If you feel unwell after the injection you will be asked to stay a little longer.
At each visit we will record details of any symptoms you experience after the injection. This is so we can adjust your dose regime depending upon your symptoms.
What happens if I miss my injection?
It is important that you try and attend your appointments as per the schedule.
If you miss your injections you may have to reduce the scheduled dose. If many treatments are missed, it may be necessary to re-start the treatment.
What side effects can occur?
The common side effects include:
- Swelling and redness at the injection site, which may be quite large in some cases.
- Nettle rash, tiredness, flushing.
- Itchy eyes and runny nose or wheezing.
Most symptoms are mild and usually settle. This does not mean that treatment would have to be stopped. You may apply ice and take an antihistamine for injection site reactions. If you are concerned please contact your general practitioner.
Serious allergic reactions (anaphylaxis) are very rare with immunotherapy treatment.
Can I have immunotherapy if I am pregnant?
We would not start immunotherapy if you are trying to conceive or are already pregnant. If you become pregnant when you are established on maintenance injections, treatment can continue.
If you have any concerns, discuss them with your immunology consultant.
Preparing for your immunotherapy
So we can ensure that your treatment is safe, please inform someone from the clinic if you:
- Have been unwell (e.g. a fever) within the 24 hours before treatment.
- Have experienced allergic symptoms within the 3-4 days before treatment.
- Develop any side effects.
- Are taking regular medications and have had any changes to these.
- Have received a vaccination within the last 7 days before treatment.
- Have any chronic conditions such as asthma, heart and/or lung disease, immune disorders.
Before your injection, avoid large meals and alcohol. We recommend that you take an antihistamine tablet (e.g. Cetirizine 10mg) one hour prior to your clinic visit/injection.
Antihistamines can be purchased from your local pharmacy who will be able to advise you on the one most suitable for you.
After the injection, please do not take any strenuous exercise for 12 hours and avoid having a hot bath. Alcohol should be avoided for at least 4 hours afterwards
Useful tips to avoid getting stung
- Move away slowly and don’t panic - avoid provoking bees and wasps.
- Wear clothing that covers most of the body (particularly the feet).
- Always wear shoes when outdoors.
- Avoid wearing bright colours, flowery prints and using products with strong scents – these can trick wasps and bees into thinking you are a flower!
- If gardening, wear long sleeves, long trousers and gloves.
- Keep food and drink covered when eating and drinking outside - wasps can crawl inside cans where they are not seen.
- Avoid flowering plants, outdoor areas where food is served, rubbish and compost
- Regularly and carefully remove any fallen fruit in your garden and keep a well-fitting lid on dustbins.
- Keep doors and windows closed
- Drive with the windows up and the air conditioner on.
Omalizumab for Chronic Urticaria
What is Urticaria?
Urticaria is a raised, itchy rash sometimes called hives or nettle rash. It is thought to be caused due to release of excessive histamine from some immune cells, which is why antihistamines are commonly used to treat this condition. There is further information available from the AllergyUK website.
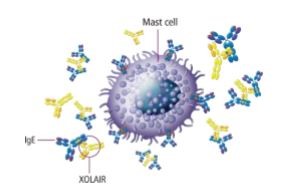
There is probably more than one mechanism or cause for chronic urticaria. Stimulation of some immune cells (called mast cells) causing release of histamine is likely to be one mechanism. Omalizumab is a man-made drug that reduces stimulation of these cells and decreases the release of histamine.
Why am I being offered Omalizumab?
You have been offered this medicine since your urticaria has not improved despite taking high doses of antihistamines and other drugs.
80-90% of people taking Omalizumab get significant benefit and about a third of patients are completely free of symptoms after 12 weeks.
It suppresses symptoms and is not a cure, so the symptoms can return once the treatment is stopped.
There is a national guideline for the use of Omalizumab. We use a questionnaire that helps us understand how much improvement there has been in your symptoms. It is important that you fill this questionnaire prior to, and intermittently during treatment, to ensure that the treatment is of benefit.
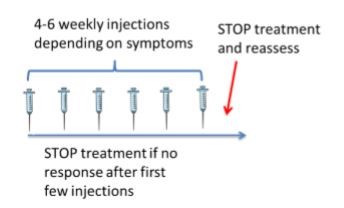
Omalizumab is licensed to be given as a series of injections every month, lasting for 6 months. Most people are able to self-administer the injections at home with support from the nursing team. In clinic we sometimes find that the injections work just as well given every 6 weeks.
We initially provide 4 doses and reassess your symptoms to see if the medicine is working. After 6 injections we will stop the treatment, but if you have a flare up of symptoms and meet the criteria again for another course of treatment, then we will restart the Omalizumab.
What are the risks of taking Omalizumab?
Some people who have had Omalizumab for urticaria have described reactions at the site of the injection, such as swelling and redness. Some patients have had an increased number of coughs and colds after starting the drug.
Are there any serious risks?
There were initial concerns that omalizumab may cause allergic reactions, but it has turned out to be a safe treatment for urticaria and reactions are very rare.
What else do I need to know?
You should not have Omalizumab if you are at risk of a worm infection (e.g. travel to some countries).
Please inform someone from the clinic if there are any changes to your other medication, if you develop any new illness, become pregnant or plan to become pregnant.
Further Information
British Association of Dermatologists www.bad.org.uk Willan House, 4 Fitzroy Square, London W1T 5HQ Tel: 0207 383 026
Novartis (who make omalizumab) Website to provide information: http://www.xolair.com/
AllergyUK www.allergyuk.org 01322 619898
Anaphylaxis is a severe allergic reaction that can be life-threatening. All patients who have a reaction like this should be seen by a doctor who can identify a possible cause and will provide a plan to avoid and also to manage allergic reactions. For more information, click here: www.anaphylaxis.org.uk
How to manage allergic reactions without an adrenaline autoinjector
How to manage allergic reactions with an Epipen
How to manage allergic reactions with a Jext
Wasp and Bee stings usually cause a large local swelling, which settles over a few days. However, if stings cause symptoms away from the site of the sting or make a person feel unwell, a specialist referral should be considered. Read more about this at the Anaphylaxis Campaign website: Insect sting allergy - the facts
Where appropriate, we offer immunotherapy (desensitisation) which is an effective treatment for bee and wasp allergy. It is a three-year course of injections. Read more about this in the allergy treatments section of this site.
Rhinitis is inflammation of the nose. Symptoms include sneezing, runny nose, blocked / stuffy nose, itching and 'post-nasal drip' (the sensation of mucus running down the back of the throat). It can occur in association with inflammation of the eyes or sinuses. Rhinitis can have several causes, such as infection, a reaction to medication, irritation by dusts, or allergy. When allergy causes rhinitis, the condition is called ‘allergic rhinitis’.
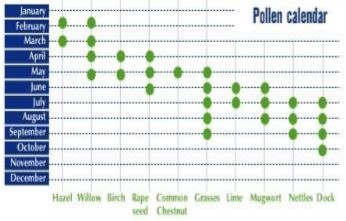
Allergic rhinitis can be seasonal or all year round:
|
Allergen |
Symptoms occur in: |
|
Grass pollen |
Summer (Summer hayfever) |
|
Tree pollen |
Spring (Spring hayfever) |
|
House dust mite |
All year round (perennial) |
|
Pets |
All year round (perennial) |
How can I avoid pollen?
- Monitor pollen forecasts daily.
- pollen count is high, when getting home remove your clothing and shower.
- Keep windows closed when indoors. Pay particular attention in early mornings when the pollen is released into the air and in the evening when the air cools and pollen begins to fall to the ground.
- Wear wraparound sunglasses and a wide brimmed hat.
- Avoid drying washing on an outdoor clothes line when the pollen count is high.
- Wipe a pets’ coat with a damp cloth to remove any pollen particles.
- Try and avoid triggers or take an antihistamine before known exposure.
How can I avoid house dust mite (HDM)?
You cannot completely avoid house dust mite! Dust mites are found mainly in the bed, soft furnishings and carpets.
- The measures outlined can help to reduce the amount of HDM exposure:
- Wash bedding often and at more than 60oc if possible.
- where possible, replace carpets with wooden floors
- Cover mattress and pillows in dust mite-proof covers.
- HDM like moist warm conditions, so let the bed air during the day and leave the window open to ventilate the room.
What if I am allergic to my pet?
Most pet owners tolerate their own pets and have problems when exposed to other pets. If you have a new pet and have been found allergic, the most effective way to reduce your symptoms will be to rehome your pet.
If this is not possible, try the following:
- Avoid close contact with your pet (e.g. cuddling, kissing, allowing to sit in your lap).
- Keep your pet away from your bedding, sofa and other areas that you frequently use.
- Where possible, replace carpets with wooden floors to reduce amount of pet fur/dust mite in the house.
How can I use my medication most effectively?
All rhinitis medication should be taken regularly to gain the maximum benefit. It is more difficult to treat symptoms that are already well established. For seasonal symptoms we recommend starting your treatment at least 2 weeks before your symptoms usually begin.
Nasal washes - Washing the nose with a saline wash can relieve symptoms and clean the nose prior to using a nasal spray. The solution can simply be sniffed up the nose, or if preferred proprietary devices are available e.g. Sinus RinseTM.
Ingredients for saline wash solution:
- 240 mls previously boiled and cooled water
- 1/4 teaspoon salt
- 1/4 teaspoon bicarbonate of soda
Antihistamines - They are available in liquid, tablet and nasal spray form. There is a large range of antihistamines, but generally daily non-sedating antihistamines are recommended e.g. cetirizine. If one does not suit you it may be worth trying a different one. Antihistamines are available over the counter in pharmacies or on prescription.
Steroid nasal spray - This is the most effective treatment for allergic rhinitis.
Taking nasal sprays
- Shake bottle well
- Look down (chin on chest)
- Using RIGHT hand for LEFT nostril put nozzle just inside nose, hold gadget pointing straight up and aim towards outside wall
- Squirt once or twice (2 different directions)
- Change hands and repeat for the other side
- DO NOT SNIFF
Nasal sprays are available over the counter or on prescription e.g. Fluticasone.
There are several types of nasal spray so you may need to try more than one to find one that works best for you.
Eye drops -Antihistamines and nasal sprays can help to ease eye symptoms.
Sodium cromoglycate eye drops can be obtained over the counter or on prescription and can also help.
Montelukast –This is another drug that blocks chemicals that cause inflammation (like antihistamines). It can be particularly useful in perennial rhinitis. It is only available on prescription.
Decongestants –These drugs e.g. Otrivine should be avoided as much as possible. If these drugs are used frequently then symptoms can get even worse and be difficult to control.
Immunotherapy –This is for patients with very severe allergic rhinitis despite taking maximum conventional medication.
Your allergy consultant or nurse will discuss this treatment with you and provide more information if they feel it is suitable in your case.
Some patients with runny nose or nasal stuffiness do not have an allergy.
What is non-allergic rhinitis?
Non-allergic rhinitis is inflammation of the inside of the nose that isn't caused by an allergy.
Symptoms of non-allergic rhinitis can include:
- a blocked nose
- a runny nose – this may be through the nostrils or down the back of the nose (catarrh)
- sneezing – although this is generally less severe than in allergic rhinitis
- mild irritation or discomfort in and around your nose
- reduced sense of smell
These symptoms can be constant or they may come and go.
What causes non-allergic rhinitis?
There are many different causes and often it is not possible to identify one cause.
There are several factors that can be associated with non-allergic rhinitis:
- Infection
- Irritants e.g. smoke, paint fumes
- Change in temperature
- Alcohol
- Spicy food
- Stress
- Some medications:
- Some blood pressure tablets (eg. those ending with a ‘pril’ such as Ramipril)
- Aspirin, Ibuprofen and other common painkillers
- Cocaine use
- Long term use of some medication available for treating blocked nose (eg. Otrivine)
- Hormonal changes e.g. pregnancy, puberty and HRT
Overuse of drugs for ‘blocked nose’
Some sprays (such as Otrivine) unblock your nose by reducing the swelling of the blood vessels in your nose. However, if they are used for longer than five to seven days at a time, they can cause the lining of your nose to swell up again. This can happen even after the original problem has resolved. If you use more decongestants in an attempt to reduce the swelling, it is likely to make the problem worse. The medical term for rhinitis caused by the overuse of nasal decongestants is rhinitis medicamentosa.
Tissue damage
Inside your nose, there are three ridges of bone covered by a layer of tissue. These layers of tissue are called turbinates. A type of rhinitis called atrophic rhinitis can occur if the turbinates become damaged.
Most cases of atrophic rhinitis in the UK occur when the turbinates are damaged or removed during surgery (sometimes it is necessary to surgically remove turbinates if they're obstructing your airflow).
Turbinates play an important role in the functioning of your nose, such as keeping the inside of your nose moist and protecting the body from being infected with bacteria. If they are damaged or removed, the remaining tissue can become inflamed, crusty, and prone to infection.
What investigations do I need?
Sometimes the symptoms will be enough to make the diagnosis clear and no tests will be required. However it is quite common to have some allergy tests to exclude this common cause of rhinitis
How can I use my medication most effectively?
All rhinitis medication should be taken regularly to gain the maximum benefit. It is more difficult to treat symptoms that are already well established.
Nasal washes - Washing the nose with a saline wash can relieve symptoms and clean the nose prior to using a nasal spray.
The solution can simply be sniffed up the nose, or if preferred proprietary devices are available e.g. Sinus RinseTM.
Ingredients for saline wash solution:
- 240 mls previously boiled and cooled water
- 1/4 teaspoon salt
- 1/4 teaspoon bicarbonate of soda
Antihistamines - Surprisingly antihistamines can sometimes be helpful.
Antihistamine nasal sprays can be obtained over-the-counter from your pharmacy or on prescription.
Anticholinergic nasal spray - These are helpful for people with primarily a runny nose.
Steroid nasal spray - This is the most effective treatment for rhinitis. Nasal sprays are available over the counter or on prescription e.g. Beclomethasone or Fluticasone. There are several types of nasal spray so you may need to try more than one to find one that works best for you.
Taking nasal sprays
- Shake bottle well
- Look down
- Using RIGHT hand for LEFT nostril put nozzle just inside nose, hold the gadget pointing straight up and aim towards outside wall
- Squirt once or twice (2 different directions)
- Change hands and repeat for the other side
- DO NOT SNIFF
Decongestants – Some cases of non-allergic rhinitis are caused by overusing nasal decongestant sprays. In these cases, the best treatment is to stop using these sprays. However, this can be difficult, particularly if you've been using them for some time.
Try not using the spray in your least congested nostril first. After seven days this nostril should open up, at which point you should try to stop using the spray in your other nostril.
Introduction
You have been referred for investigation of a suspected allergy. As part of this investigation, you may be offered an oral challenge. This leaflet aims to tell you what to expect.
What is an allergy?
Adverse reactions to foods can be allergic and non-allergic (intolerance). Allergic reactions are caused by the immune system.
What happens after I have had a reaction?
You will be referred as an outpatient to a centre specialising in allergy, where you may have a blood and / or skin prick test. This can help to identify what caused your reaction. If your test results are positive, you will be advised to avoid that particular food.
Often if the reaction was typical of an allergic reaction you may be advised to avoid that food, even if the test results are negative.
If the symptoms were not typical, the tests were negative and you would like to reintroduce that food back into your diet, then a ‘challenge’ may be offered.
A challenge is the best way to determine how you will react to a particular food.
What happens in a challenge?
An appointment will be made for you to attend the allergy challenge clinic.
The challenge is performed in hospital, in order that you can be closely monitored. You will be asked to bring with you the food that may be causing your reaction. You will be asked to sign a consent form.
You may have an allergy skin prick test prior to the challenge.
Increasing amounts of the food are given over time, with close observation for reactions. Observations may include pulse, blood pressure and peak flow (a breathing test).
The exact duration and number of stages will depend on previous reactions and symptoms during your test, but typically a challenge to a food will take 2 - 3 hours.
The amount of food required will vary, but the aim is to have taken a sufficient quantity to exclude allergy.
After the final amount, you will be observed for at least 1hr before you can be discharged.
Challenges carry a risk. If you have any symptoms, however mild, let the doctor or nurse know. We can then treat the symptoms quickly and prevent the reaction progressing. A cannula may sometimes be placed in a vein. Such symptoms usually occur within an hour of exposure to the food. The allergy team will write to your GP advising them of the outcome.
What kind of reaction may I have?
The most common reactions are:
- Flushing or rash
- Itching
- Lip swelling and facial swelling
Less common reactions are:
- Wheezing
- Itchy watery eyes and nose
- Nausea
- Rarely more severe reactions can occur causing faintness and anaphylaxis.
What happens if I react to the food?
The challenge will be stopped and treatment given if necessary.
Rarely ward or emergency department admission may be required if a severe reaction occurs, in order to monitor you closely and provide additional treatment.
You will be advised to avoid this food in the future.
What do I need to do before the challenge?
- Bring the food for the challenge
- Stop taking anti-histamines for 5 days before appointment
- Avoid aspirin or similar non-steroidal anti-inflammatory drugs on day of the challenge
- Expect to be in outpatients for the majority of the morning
- If possible bring someone with you
- Eat and drink normally prior to the challenge
Inform a member of the immunology team if you:
- are taking prednisolone
- are taking beta blockers eg atenolol
- are unwell
- have asthma and are using your blue inhaler more frequently
What happens if I become unwell after I leave hospital?
Treat reactions according to your management sheet
Make a note of the symptoms and when they happened and let the immunology team know
Further Information
AllergyUK www.allergyuk.org 01322 619898
The Anaphylaxis Campaign 1 Alexandra Road Farnborough Hampshire. GU14 6BU 01252 542029 www.anaphylaxis.org.uk
The MedicAlert Foundation 1 Bridge Wharf 156 Caledonian Road London N1 9UU Monday to Friday 9am to 5pm Freephone 0800 581420 (UK) or 1800 581420 (Ireland) Fax 020 7278 0647 info@medicalert.org.uk www.medicalert.org.uk
The respiratory specialists in Royal Stoke University Hospital manage asthma. You can find information about this service on the ‘adult asthma’ page of the UHNM website.
Introduction
You have been referred for investigation of a suspected drug or vaccine allergy. As part of this investigation, you may be offered an oral drug or vaccine challenge. This leaflet aims to tell you what to expect.
What happens after I have had a severe reaction?
You will be referred to a centre specialising in allergy as an outpatient where you may have a blood and / or skin prick test. This can help to identify which drug or drugs caused your reaction. If your test results are positive, you will be advised to avoid that particular drug and advised to wear a medical alert emblem at all times (see Further Information).
Most often if there is a possibility that someone is allergic to a particular drug then they can just avoid it. However, sometimes it is important that patients are able to use a particular drug if possible e.g. antibiotic. If it is important that you know whether it is safe for you to take a particular drug and the tests for allergy are negative then a ‘challenge’ may be offered. This is the best way to determine how you will react to a drug or vaccine.
What happens in a challenge?
An appointment will be made for you to attend the allergy challenge clinic.
Drug challenges carry a risk. We do the challenge in hospital to minimise the risk. You will be asked to sign a consent form.
- You may have an allergy skin prick test prior to the challenge.
- Increasing doses of the drug or vaccine are given over time, with close observation for reactions. Observations will include pulse, blood pressure and peak flow (a breathing test).
- The exact duration and number of stages will depend on previous reactions and symptoms during your test, but typically a challenge to one drug will take 2 - 3 hours.
- The amount of drug required will vary, but the aim is to have taken one standard dose of the drug by the end of the challenge.
- After the final dose, you will be observed for up to 2 hours before you can be discharged.
- Sometimes, e.g. antibiotics, you are advised to complete a course of treatment at home at the end of the challenge. This is to look for delayed reactions.
If you have any symptoms, however mild, let the doctor or nurse know. We can then treat the symptoms quickly and prevent the reaction progressing. A cannula may sometimes be placed in a vein.
If you have no reaction during the challenge, the allergy team will write to your GP advising them that you are able to take that particular drug.
What kind of reaction may I have?
The most common reactions are:
- Flushing or rash
- Itching
- Lip swelling and facial swelling
Less common reactions are:
- Wheezing
- Itchy watery eyes and nose
- Nausea
- Rarely more severe reactions can occur causing faintness and anaphylaxis.
What happens if I react to the drug or vaccine?
The challenge will be stopped and treatment given if necessary.
Ward or A&E admission may be required if a severe reaction occurs in order to monitor you closely and provide additional treatment.
You will be advised to avoid this drug completely.
What do I need to do before the challenge?
- Stop taking anti-histamines for 5 days before the appointment.
- Avoid aspirin or similar non-steroidal anti-inflammatory drugs on day of the challenge
- Expect to be in the outpatients clinic for the majority of the morning
- Eat and drink normally on the day of the challenge
If you are not sure about this please ask.
Inform a member of the immunology team if you:
- are taking prednisolone
- are taking beta blockers eg atenolol
- are unwell
- have asthma and are using your blue inhaler more frequently
What happens if I become unwell after I leave hospital?
- Treat reactions according to your management sheet
- Make a note of the symptoms and when they happened and let the immunology team know
Further Information
AllergyUK www.allergyuk.org 01322 619898
The Anaphylaxis Campaign 1 Alexandra Road Farnborough Hampshire. GU14 6BU 01252 542029 www.anaphylaxis.org.uk
The MedicAlert Foundation 1 Bridge Wharf 156 Caledonian Road London N1 9UU Monday to Friday 9am to 5pm Freephone 0800 581420 (UK) or 1800 581420 (Ireland) Fax 020 7278 0647 info@medicalert.org.uk www.medicalert.org.uk
What is immunotherapy?
Immunotherapy, often referred to as desensitisation, is the only proven treatment that can reduce allergy symptoms in the long-term. Immunotherapy is a well-established treatment for certain severe allergies, and involves the administration of gradually increasing doses of allergen extracts over a period of years. It is given to patients by injection or drops/tablets under the tongue (sublingual).
On average people with hay fever have about 30% improvement in symptoms following immunotherapy. The success of the treatment can vary between individuals. Some people will be almost free of symptoms, most will still need some medication, and a small number of patients will not show any improvement at all. We will review your symptoms after the first year.
Can everyone have immunotherapy?
No. Not all individuals with hay fever are suitable for this treatment. Your consultant will decide whether or not you are likely to benefit from this treatment.
Immunotherapy is not recommended in patients with poorly controlled asthma as they are more likely to experience severe reactions. It should also not be commenced during pregnancy.
Sublingual Immunotherapy (SLIT)
How is the treatment given?
This treatment involves a daily dose of allergen being administered as a tablet or drops under the tongue. It is important to take the medication every day. The first dose is given in hospital and subsequent doses at home. An improvement in symptoms occurs in the first season, but it is necessary to continue for 3 years to get lasting benefit.
Side effects
Common
Local symptoms such as itching in the mouth, but this improves during the first few weeks.
Indigestion symptoms
Throat discomfort
Rhinitis symptoms e.g runny nose
Rare
Tightness of the chest or wheeze
Anaphylaxis
Subcutaneous Immunotherapy
Rarely some people may not be able to have sublingual treatment and then subcutaneous treatment may be offered.
How is the treatment given?
Immunotherapy should take place before the tree or grass pollen season starts. The injection has to be administered in hospital so you can be closely monitored.
Immunotherapy involves a total of 6 injections per year being administered just under the skin on your arm. The dose will be slowly increased every 7-14 days for 3 injections and then 3 further injections every 14-28 days. Treatment is continued for 3 years. You will have to be observed for at least 1 hour after the injection. 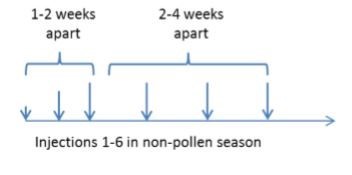
What you should know about the injections.
You should let us know if you have:
- been feeling unwell in the 24 hours preceding the treatment
- started new medication or have had vaccinations since your last injection.
You should not eat a large meal immediately before the injection is administered and limit alcohol consumption
You should not take any strenuous exercise for 12 hours after the injection.
What happens if I miss my injection?
It is important that you try and attend your appointments as per the schedule.
If you are 2 weeks late for having an injection, the treatment regime would have to re-start from the beginning.
Side effects
Common
Redness and slight swelling at the injection site. These can be treated by applying ice packs and/or taking an antihistamine (e.g. Cetirizine 10 mg tablet)
Feeling tired and lethargic– this is often temporary and should resolve within a few hours
Less common
Symptoms of hay fever or nettle rash/ hives (also called urticaria).
Rare
Chest tightness and wheeze
Anaphylactic shock
If you develop any side effects, please inform the allergy team.