Taking Moviprep oral bowel cleansing agents safely and effectively for colonoscopy/flexible sigmoidoscopy
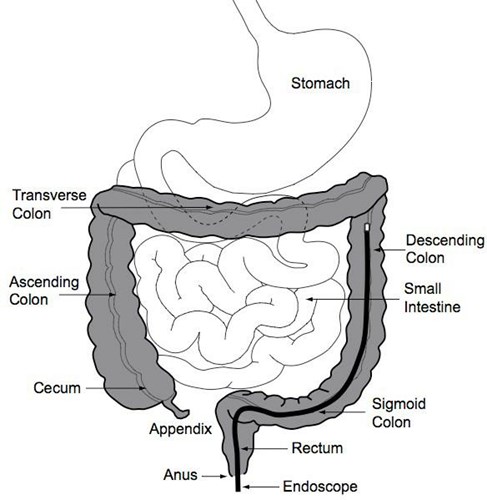
What is a colonoscopy/flexible sigmoidoscopy?
This is where a soft, flexible tube with a camera at the end is passed through your back passage (anus) and up inside your bowel by a specially trained doctor or nurse.
You should have received the procedure leaflet with your appointment letter which explains the procedure in more detail. If you have not received a copy of this, please ask us for one.
Why do I need to prepare for this procedure?
Your bowel needs to be empty for the procedure so that the doctor or specialist nurse can see the lining of your bowel.
To achieve this you will need to alter your diet and take specific preparations for a few days before the procedure.
The changes are explained in this leaflet.
What is bowel prep?
You have been supplied with an oral preparation which is a bowel cleansing agent (sometimes called “bowel prep”).
The purpose of this is to clear out your bowels and ensure safety and effectiveness of the planned endoscopic procedure.
There is a risk of developing dehydration, low blood pressure or kidney problems with this medication.
Frequently Asked Questions (FAQs)
Q: How long does the procedure take?
A: A colonoscopy usually takes between 10 and 45 minutes. A flexible-sigmoidoscopy takes between
10 and 20 minutes. You may be in the department for approximately 3 hours.
Q: Does it hurt?
A: Sometimes patients find the test painful, gas and air (Entonox) or sedation is available to use for pain relief if needed.
Q: Can I take my tablets as normal?
A: Yes unless you have been instructed otherwise see page 4, 5, 8 & 12. If your tablets need to be taken at the same time you are drinking the Moviprep please
take them at least one hour before or at least one hour after drinking Moviprep. Please see separate patient procedure information that will be sent with your appointment letter for more advice e.g. Diabetics,
those on antiplatelets and anticoagulants.
Q: Will I be asleep for this procedure?
A: No. Gas and air (Entonox) or sedation is available (if your circumstances permit).
You will be awake throughout the procedure.
Points to Remember
You will experience watery bowel movements so stay close to a toilet.
If you have not had your bowels open after taking the solution please seek medical advice.
If your health has deteriorated since seeing the doctor or specialist nurse in clinic, please call the
consultants who referred you for this test or your GP.
On the day of your test
IT IS IMPORTANT THAT YOU ONLY DRINK CLEAR (NO MILK) FLUIDS UP TO 2 HOURS BEFORE THE TEST.
After your test, you will be advised when to return to your usual diet and medication.
The person prescribing the oral bowel cleansing agent will have assessed your risk and identified the most appropriate medication for you.
You may also require a recent blood test to check your kidney function.
The following conditions apply in all cases:
- The bowel prep will cause diarrhoea and urgency so you will need to stay close to toilet facilities.
- If after taking your bowel preparation you have not had your bowels open within 7-8 hours after taking the last sachet of Moviprep, please seek medical advice as soon as possible.
- Make sure that you drink plenty of water up
to 2 hours before your test as the bowel prep can cause dehydration.
- Do not drink dark coloured juices or milk.
- If you experience symptoms of dizziness or light headedness (particularly on standing up), thirst or reduction in passing urine, then you may be dehydrated and should seek medical attention.
All bowel cleansing agents cause diarrhoea so if regular medication is required, it should be taken either one hour or more before taking the cleansing agent. Or, it should be taken 1 hour or more after taking the cleansing agent.
Please tell the nursing staff as soon as possible on the number at the end of the leaflet if you:
- Take any medicines to thin the blood or to prevent blood from clotting (anticoagulants or antiplatelets, such as warfarin, rivaroxaban, dalteparin or clopidogrel).
- Have diabetes (contact your nurse specialist).
- Have an allergy to Moviprep or its ingredients.
If you only take low dose 75mg aspirin, you do not need to call.
Do not take any other medication at the same time as you are taking the bowel prep.
Please let us know if you are taking any regular medicines at your pre-assessment appointment (including anything you buy yourself over the counter or any herbal or homeopathic medicines).
Female Patients diarrhoea can make oral contraceptive pill less effective. Continue with the pill and use extra precautions for the next 7 days.
Refer to the manufacturer’s instructions when taking your preparation for a list of ingredients and allergies.
Please adhere to the low residue diet advice sheet as certain foods can affect the outcome of your test and may result in a failed test.
How to take Moviprep
- About 6.00pm mix your first litre of MOVIPREP.
- Empty the contents of ONE sachet A and ONE sachet B in to a jug and add 1 litre (1¾ pints) of cold water and stir until dissolved. (if desired, cordial can be added to taste).
- Drink 250ml (½ pint) of Moviprep mixture every 15-30 minutes until you have drunk it all (usually over about 1-2 hours - no need to rush).
- It is important to drink an additional 500ml (1 pint) of water or fluid of your choice (No Milk).
- At 8.00am on the morning of the appointment, please mix
the remaining sachets of Moviprep following the instructions above.
- Drink 250ml (½ pint) of Moviprep mixture every 15-30 minutes until you have drunk it all (usually over about 1-2 hours) – no need to rush.
- It is important to drink an additional 500ml (1 pint) of water/ clear fluids in the morning (No Milk).
You will experience watery bowel movements so stay close to a toilet. If you have not had your bowels open after taking the solution please seek medical advice.
Adult Moviprep instructions for an afternoon appointment
There may be medicines which you are asked to stop taking and these may include:
- Heart/Blood pressure tablets e.g. Lisinopril, Ramipril, Perindopril, Captopril, Losartan, Candesartan, Irbesartan, Valsartan;
- Diuretics (Water tablets) e.g. Furosemide,
Bendroflumethiazide , Spironolactone, Amiloride, Co-Amilofruse, Bumetanide, Metolazone,
Indapamide, Eplerenone;
- Anti-inflammatory drugs e.g. Ibuprofen, Naproxen
- Tolvaptan: Used for progressive Autosomal Dominant Polycystic Kidney disease or conditions causing low sodium.
Your medication will have been discussed and advice given during your clinic or pre-assessment appointment.
Dietary Management – Low Residue Diet
Three days before your procedure you should start to eat a low residue (fibre) diet. This reduces the stool residue in the bowel. The main sources of fibre in the diet are cereal products, vegetables, seeds and fruits, so these foods need to be reduced.
It is important to have regular meals and a varied diet which includes foods such as meat, poultry, fish, eggs and dairy products (milk, cheese, yoghurt).
It is important to drink plenty of fluid and at least 8-10 cups of water, black tea/coffee, or squash per day. This helps to flush the bowel contents out and will improve the effect of the bowel preparation. It will also prevent you
from becoming dehydrated.
Suggested meals you can eat that are low residue.
Vegan option available on request from Endoscopy
MOVIPREP INSTRUCTIONS
STEP 1
Empty the contents of 1 sachet A and 1 sachet B in to a 1 litre Jug of water.
STEP 2
Stir until the solution is clear
STEP 3
Drink 1 glassful 250ml (¼ litre or
½ pint) of Moviprep every 15 minutes until you have drunk it all.
You can eat any combination of the following:
Adult Moviprep instructions for a morning appointment
Please adhere to the low residue diet advice sheet as certain foods can affect the outcome of your test and may result in a failed test.
How to take Moviprep
- At 6pm empty the contents of ONE sachet A and ONE sachet B in to a jug and add 1 litre (1¾ pints) of cold water and stir until dissolved. (if desired, cordial can be added to taste).
- Drink 250ml (½ pint) of Moviprep mixture every 15-30 minutes until you have drunk it all (usually over about 1-2 hours - no need to rush).
- It is important to drink an additional 500ml (1 pint) of water or fluid of your choice (No Milk).
- Make up your second litre of Moviprep as above and continue to drink, followed by 500ml water or fluid of your choice (No Milk).
- Allow 2 hours after taking the second litre for the Moviprep to work.
- Go to bed when you stop going to the toilet (e.g. 11.00pm or 12.00 Midnight).
You will experience watery bowel movements so stay close to a toilet. If you have not had your bowels open after taking the solution please seek medical advice.
ON THE DAY OF YOUR TEST IT IS IMPORTANT THAT YOU ONLY DRINK CLEAR (NO MILK) FLUIDS UP TO 2 HOURS BEFORE THE TEST
Q: How can I make the Moviprep more palatable?
A: It is important to sip the Moviprep and not gulp it down to reduce nausea. A straw is sometimes helpful to drink the Moviprep with and you can add cordial (not blackcurrant) to taste if you prefer. Chilling your Moviprep solution can also sometimes help.
Q: What shall I wear to attend the procedure?
A: You will be asked to wear a hospital gown and dignity shorts. You can bring your own dressing gown and slippers.
If you have any further questions
Please telephone the Endoscopy Booking Office on 01782 676010, or 01782 675713 this is a voice message facility so please leave your name, hospital number and contact number.
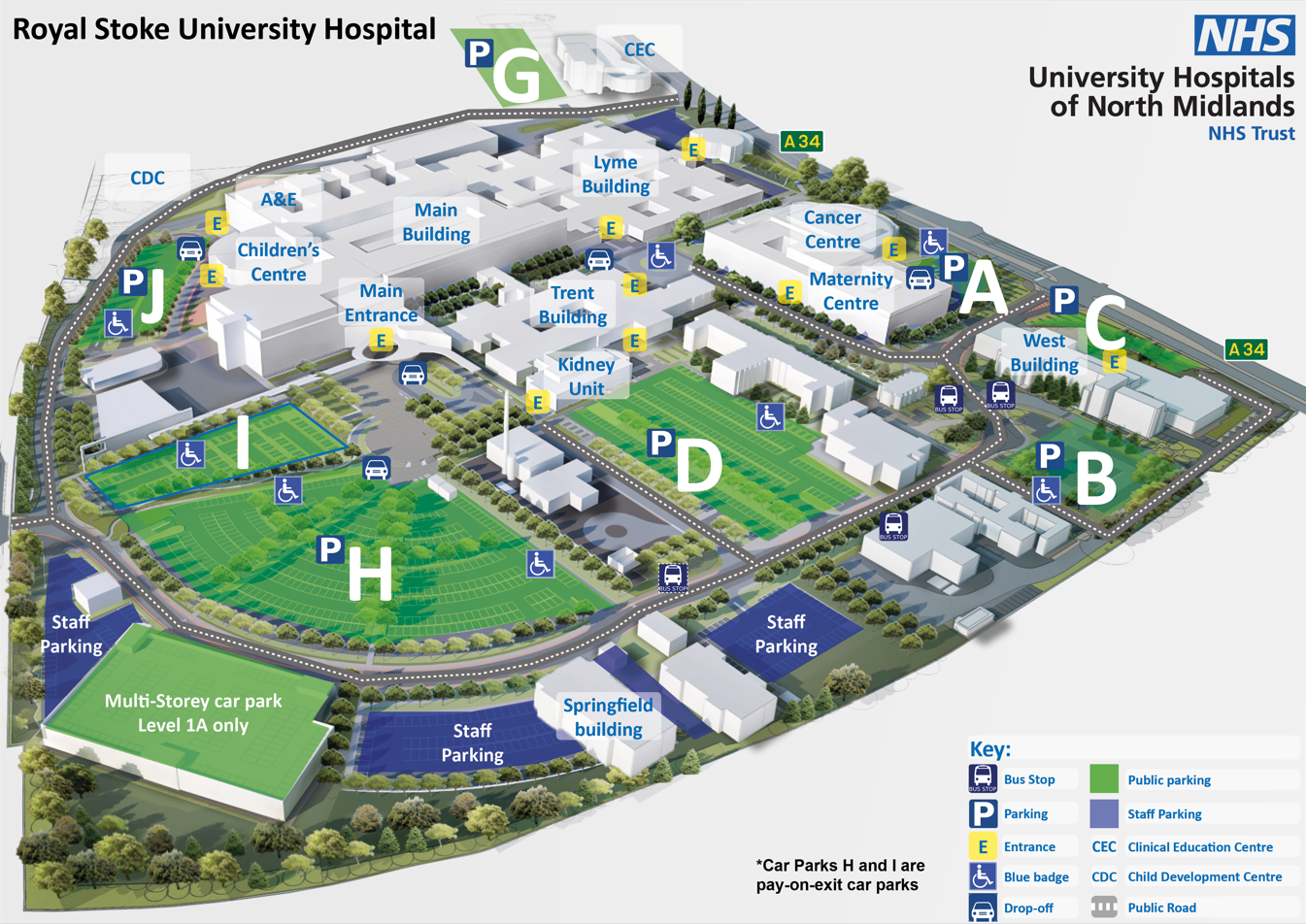
 Please note, car parking charges apply. There is a shuttle bus service running between Royal Stoke and County Hospital. Please call 01782 824232 to arrange a place on the bus.
Please note, car parking charges apply. There is a shuttle bus service running between Royal Stoke and County Hospital. Please call 01782 824232 to arrange a place on the bus.