Radiotherapy treatments are routinely delivered every weekday Mon-Fri between 8.30AM-4.30PM. It is important that patients keep to their appointment schedules as much as possible, however if they are feeling unwell or unable to attend then they should contact their treatment machine directly, the telephone number can be found on the appointment card given to them at their CT scan or in the contacts section at the end of this page. Patients are advised to discuss any plans for holidays with their consultant or radiographer as soon as possible. In the Radiotherapy department at the Royal Stoke we do work most public bank holidays; we will make sure that people are aware of the dates that they need to attend. Some gaps in treatment may be allowed when machines are serviced, machines breakdown or during some public holidays. Any necessary adjustments will be made to treatment to account for these. Very occasionally we may ask patients to attend for treatment on a weekend but this will be made well aware to the people this may affect.
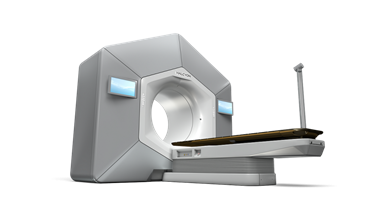
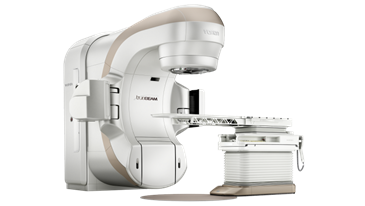
Radiotherapy is delivered by Linear Accelerators (Linacs). We have 2 different types of Linacs in the Radiotherapy Department at the Royal Stoke, with all 4 machines doing the same job and having state-of-the art up-to-date technology
Halcyon treatment machine ©Varian



Truebeam treatment machine ©Varian

The number of treatments on the linac depends on each patient's condition. It can be anything from 1 to 37 treatments and each treatment can take anything from 5 to 60 minutes. Most of the time is taken in getting the patient in the right position for the treatment. The delivery of the treatment itself is similar to an x-ray and very quick & painless with nothing to see or feel. All we need the patient to do is keep very still and breathe normally.
No-one is allowed to be in the room while a patient is receiving radiotherapy, but the Therapy Radiographers can see and hear them at all times through CCTV & intercoms. The CCTV is never recorded; it is just a live feed so that the patient can alert the staff if needed. The machine can always be stopped if necessary and the staff can go into the room to attend to the person. The Radiotherapy Department at UHNM is a very busy unit, but wherever possible the staff do try to offer patients’ appointments at times of day that work around them in order for patients to make it easier to organise their lives around the treatment.
External radiotherapy does not make people radioactive so it is perfectly safe for people to be around others (including children) during and after their course of treatment. However it may be advisable to avoid being close to people who are unwell, especially if the patient has had/is having chemotherapy. It is also very important that patients are not and do not become pregnant during their course of radiotherapy. If anyone is concerned regarding this please discuss this with a member of staff.
Radiotherapy is delivered by a team of suitably trained radiographers, both male and female. We are also a teaching hospital and regularly have student radiographers in the department who are supervised by trained staff. Chaperones can be used if wanted; please make a member of staff aware if the patient would like this.
Patients have daily contact with the radiographers who look after them while they are attending for treatment and can answer most questions that they may have. During the course of treatment patients will also normally have the opportunity to speak to a nurse or a doctor about any other concerns or specific aspects of their care.