Ward 225 and 226, Main Building, Floor 2, Royal Stoke University Hospital
Ward 225: 01782 676225
Ward 226: 01782 676226
Orthopaedics is the diagnosis and treatment of bone, joints and skeleton-related problems. University Hospitals of North Midlands prides itself in having a top quality orthopaedic surgery department. The consultant orthopaedic team are experts in their field and provide a comprehensive service in trauma surgery and elective orthopaedic procedures.
Our orthopaedic consultants specialise in various parts of the body such as hips, knees, ankles, hands, feet, shoulders and elbows and deal with anything from a broken bone to a hip replacement and carpal tunnel syndrome to spinal surgery. Some of our consultants also deal especially with children's fractures and orthopaedic conditions and sports injuries.
Ward 225 and 226, Main Building, Floor 2, Royal Stoke University Hospital
Ward 225: 01782 676225
Ward 226: 01782 676226
Carpal tunnel syndrome is a condition where there is increased pressure on the nerve that crosses the front of the wrist (the median nerve). This nerve runs in a tight tunnel together with the tendons that bend the fingers. If the tunnel becomes too tight, this can compress the nerve usually causing pain, tingling or numbness in the thumb index and middle fingers. These symptoms can be worse at night.
Carpal tunnel syndrome is usually more common in women and can be associated with other factors such as arthritis, pregnancy, wrist fractures, diabetes or thyroid problems. Most sufferers have no underlying cause, but if your symptoms are less clear, your doctor may recommend further tests to confirm the diagnosis. Your consultant has recommended an operation called a Carpal Tunnel Release. It is your decision to go ahead with the surgery or not. This text will give you enough information about the benefits and risks so that you can make an informed decision. If you have any questions that this document does not answer, you should ask your surgeon or any member of the healthcare team.
The main benefit is to relieve the pain, tingling and numbness in the hand.
If the symptoms are mild a wrist support worn at night can help. Also a small injection of steroid in the tunnel may help to reduce some of the symptoms on a temporary basis. If the symptoms are severe and these measures have failed, then surgery is usually recommended.
Symptoms may improve if there is an underlying cause that is treated. In those with no underlying cause, symptoms usually continue, but can get better or worse for no known reason. If the pressure on the nerve is severe and the condition is left untreated the nerve can be permanently damaged. This can result in weakness of the thumb muscles and permanent numbness. Surgery done at this stage may not be able to reverse the damage already caused
This involves a small cut in the palm of your hand. They will then cut the tight carpal ligament (flexor retinaculum) that forms the roof of the carpal tunnel. This relieves the pressure in the tunnel and stops the nerve being compressed. The wound is then closed and a firm dressing put on. If you have the surgery under local anaesthetic, then you will be able to leave within an hour or two after the surgery.
The healthcare team will try to make your operation as safe as possible, however somecomplications can happen.
1. Complications of local anaesthesia
Local anesthetic is a drug that is injected into the tissues to make them numb. This temporarily stops the nerves working so that you do not feel the pain of the surgery. This can sting or burn for a few seconds and then the area goes numb. You may still feel pressure or touch. The local anaesthetic works for a few hours and then the area returns to normal. If you are unsure about a local anesthetic you need to discuss options with your surgeon. These are possible complications:-
• Not enough pain relief – this is corrected by injection some more around the area.
• Allergy – this is rare, but let someone know if you have had problems in the past.
• Bleeding – the needle can touch a small blood vessel, so a small bruise may occur.
• Permanent nerve damage – rare, but the anaesthetic can have a longer effect that expected.
• Absorption into the blood stream – if the local anesthetic is accidentally injected into the blood stream, then there may be stronger reactions temporarily affecting the heart and brain which can be serious – the dose is always limited to limit these risks.
2. Complications of any operation
• Pain – this happens with any surgery. This will be controlled with medication and it is important that you take this. However the cut is small and usually not very painful.
• Infection in the wound – this usually settles with antibiotics, but may require further surgery.
• Scarring – the cut is usually lies within one of the wrist creases and usually becomes invisible over time.
3. Specific complications
• Numbness in the fingers or palm – caused by damage to the median nerve. This can be temporary (1 in 100) or permanent (1 in 600)
• Tenderness of the scar – this is very common and usually settles in about six weeks. However mild tenderness can last for a long time (1 in 5)
• Aching in your wrist when using your hand (1 in 25)
• Continued mild numbness (1in 4)
4. Even though the operation is usually a success, the nerve may have been damaged by pressure.
There may be some return of the numbness and pain which is caused by scar tissue(1 in 17). You may need another operation to release the nerve again. Occasionally there may be severe pain, stiffness and loss of use of the hand (complex regional pain syndrome) – this is rare and the cause is not known. Further treatment may be required including pain relief and physiotherapy, but can take months or years to get better.
After the operation you will be transferred to a recovery waiting area. If you are worried about anything before you go home ask a member of the healthcare team. At home you should keep you hand elevated and bandaged for the first few days. It is important to exercise your fingers, elbow and shoulders to prevent stiffness. After the first few days the dressing can be reduced, but keep the wound area dry and clean until the stitches are removed. Do not drive until you are confident of controlling your vehicle – always check with your insurance company first. You should be reviewed by the consultant approximately 6 -10 weeks after your surgery – you can discuss any issues at this time.
In 3 out of 4 people symptoms of carpal tunnel syndrome recover quickly after the operation – for others recovery is slower or less complete. Your symptoms may continue to improve for up to six months or even longer. If you had wasting of your hand muscles before the operation, this is unlikely to get better. However, the procedure should improve the pain and prevent further nerve damage. Overall, the operation is a success in 7 out of 8 people.
Carpal tunnel syndrome is a troublesome condition which usually gets better with an operation. This is a monitor procedure performed under local anaesthetic. Surgery is usually safe and effective. However complications can happen and you need to know about them to help you make an informed decision. Knowing about them will also help to detect and treat any problems early.
The Patient Advice and Liaison Service (PALS) would be please to hear any comments or suggestions that you may have about our services. They can offer confidential advice and support. They can be contacted on 01782 552814 or via email at patient.advice@uhns.nhs.uk
You can also get further information from:
• www.aboutmyhealth.org – for support and information
• Arthritis research campaign, or 0870 850500
• NHS direct on 0845 46 47
If you have any other concerns or queries then please contact a member of our clinical Governance team on 01782 555155
Dupuytren’s Contracture and fasciectomy
This booklet provides information for you and your family regarding Dupuytren’s Contracture. Your decision on treatment must be based upon weighing the benefits against any risks. If you have any questions as you read through this leaflet then ask the doctor, nurse or therapist at your next visit. You may find it helpful to make a note of your questions before
you see the doctor or nurse.
Dupuytren’s disease is a condition where scar-like tissue forms just beneath the skin of the fingers and the palm of the hand. Over time, this fibrous tissue can contract and force one or more fingers to curl up into the palm. This is known as Dupuytren’s contracture (see figure 1)
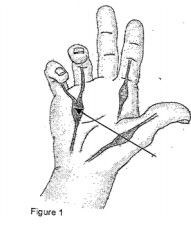
Your surgeon may have recommended a Dupuytren’s fasciectomy operation. However, it is your decision to go ahead with the operation or not. This text will give YOU enough information about the benefits and risks so you can make an informed decision.
If you have any questions that this document does not answer, you should ask your surgeon or any member of the healthcare team.
The reason why fibrous nodules and bands of tissue form is not fully understood. It used to be thought that the disease was caused by heavy manual work, but this is not the case. Dupuytren’s contracture is more common in men than in women, and it tends to run in families. It is sometimes associated with diabetes, liver disease or smoking. However, most sufferers have no particular risk factors, if one or more fingers develop contractures that interfere with the function of their hand, surgery may be recommended.
After surgery, you should be able to make better use of your hand and straighten the affected fingers further.
The only effective treatment for Dupuytren’s contracture is surgery. There is no effective drug treatment available. Wearing a splint on the affected hand does not stop the disease from getting worse
Although surgery is not essential, Dupuytren’s contracture does not get better without it. The condition will often get slowly worse with time and can result in one or more fingers being held bent into the palm. If this is left untreated, the finger joints themselves may become permanently stiff and an operation at this stage is less likely to be a success. Sometimes the only option for a very stiff and contracted finger is amputation.
You should remove any rings from your hand before you come into hospital. The type of surgery needed depends on the position and severity of the Dupuytren’s contracture, the condition of the skin and if there has been any previous surgery. Surgery can range from, simply cutting a fibrous band in the palm under local anaesthetic to removing all of the affected skin and replacing it with skin grafts. Before the operation, your
surgeon will discuss with you the type of surgery you are likely to need.
• Lifestyle changes
If you smoke, try to stop smoking now. There is strong evidence that stopping smoking several weeks or more before an anaesthetic reduces your chances of getting complications. Further contractures are more likely to happen if you continue to smoke after your operation.
If you are overweight, losing weight will reduce your chances of developing complications.
• Medication
You should continue your normal medication unless you are told otherwise. If you are on Warfarin, you will need to stop taking it before the operation. Make sure your surgeon is aware you are on Warfarin and follow the advice about stopping it.
The healthcare team will try to make your operation as safe as possible. However, complications can happen. Some of these can be serious. You should ask your doctor if there is anything you do not understand. Any numbers which relate to risk are from studies of patients having this operation. Your doctor may be able to tell you if the risk of a complication is higher or lower for you. The complications fall into three categories.
1. Complications of anaesthesia
2. General complications of any operation
3. Specific complications of this operation
Your anaesthetist will be able to discuss with you the risks of having an anaesthetic.
• Pain, which happens with every operation. Local anaesthetic may be injected into your hand during the operation to help relieve any pain you may feel after the operation. The healthcare team will give you medication to control the pain.
• Scarring of the skin.
• Infection in the surgical wound. This is uncommon and usually settles with a course of antibiotics.
• Injury to the small arteries in a finger. If both the main arteries to a finger get damaged, you may lose the finger. This is very rare.
• Incomplete correction of the Dupuytren’s contracture due to loss of movement of the finger joints. Your surgeon will let you know before the operation how much correction you can expect from Surgery.
• Stiffness of the finger Joints The risk increases if you have arthritis in your fingers.
• Numbness in the fingers operated on. The small nerves in the fingers often pass near or even through the fibrous Dupuytren’s tissue so some damage to the nerves is possible. This usually improves with time but you may not completely recover normal feeling. Your fingers may also be sensitive to cold.
• Wound-healing problems. The wounds can be quite moist and sticky for a couple of weeks after the operation. Sometimes a small area of skin dies. This is not usually a cause for concern and the wounds generally heal well.
• Severe pain, stiffness and loss of use of the hand (Complex Regional Pain Syndrome). This is rare and the cause is not known. If this happens, you may need further treatment including painkillers and physiotherapy. The hand can take months or years to get better.
In hospital
After the operation you will be transferred to the recovery area and then to the day-case Ward. Your hand will be wrapped in a bandage and you will need to keep it lifted up in a sling. You should be able to go home later on the same day. A responsible adult should take you home in a car or taxi, and stay with you for at least 24 hours, regardless of whether you have had the surgery under local anaesthetic or general anaesthetic. You will need support for a few days.
Follow up
You should have a review with your surgeon 1-2 weeks after the surgery. You will then be seen by the occupational therapists for splintage and stretching exercises. Depending on the severity of your contracture, you may need to see the therapists on a weekly basis for the first few weeks. It is important that you follow any instructions carefully to get the best result from the operation. The stitches should be removed after about 2 weeks and a further review with the consultant a few weeks after then.
If you are worried about anything once you are at home contact a member of the healthcare team on the phone number they give you. They should be able to reassure you or arrange for you to have a check-up.
Returning to normal activities
Your surgeon and occupational therapist will advise you when you can return to normal activities. You will be seen in the outpatient clinic to check that the wounds are healing satisfactorily. Do not drive until you are confident about controlling your vehicle and always check with your insurance company first.
The future
It can take some time for your hand to settle down after surgery. Slight stiffness of the finger joints is fairly common. The scars can be fairly thick at first but will gradually become less obvious.
Dupuytren’s disease will probably come back in most people eventually, but will not always need further surgery. This is usually due to new fibrous bands and nodules forming.
We want you to be our partner in care. Please try to help by:
• Providing full information on your health history and related matters
• Following the advice given to you
• Accepting responsibility if you refuse treatment or medical advice
• Taking reasonable care of your own property and respecting the property of other people in hospital
• Keeping appointments and giving adequate notice if unable to do so
• Switching off your mobile phone when in hospital
• Not smoking except in designated areas
• Ensuring reasonable and responsible behaviour by yourself and your visitors
• Please return any equipment when you have finished with them
If you have any questions, which are not answered by this booklet, then please don’t hesitate to ask your doctor or one of the nursing staff.
The Patient Advice and Liaison Service would be pleased to offer confidential advice and support if you have any concerns. PALS can be contacted on 01782 552814 or Email patient.advice@uhns.nhs.uk
University Hospital of North Staffordshire Internet Site - www.uhnm.nhs.uk
Fracture Neck of Femur (Broken Hip)
Having broken your hip and come into hospital, we will look after you in the best possible way. This patient information booklet outlines the various
stages of the pathway of care, right from coming to the Emergency department to discharge from this hospital. Ours is a team involving various disciplines, who come together to ensure a smooth journey through this period.
You will have been brought to the Emergency department because you
have hurt your hip. In order for us to decide what is wrong with your hip.
and how best to treat it, we need to organize some tests.
These include:
• X-ray of the hip (to see the type of fracture and the best way of treating it).
• X-ray of your chest (to check for any heart or lung problem).
• ECG (Heart tracing).
• Blood tests.
These tests help us decide if you need an operation, and if so, which type
of operation. During this period, we will keep you as comfortable as possible with pain killers and other medication. We also need to start you on a drip to maintain your fluids.
We will arrange for you to be transferred to one of our specialist trauma
wards (12, 19 and 24), as soon as a bed is available (usually less than 4
hours of coming to the emergency department). On the ward/Care before your operation. You will have a full medical assessment of your condition to determine your general health and your fitness for an operation. We may, at times, have to run some more tests, seek advice from other specialties and give you some treatment, to help you get strong enough to have the operation. We would like to help you get safely back to your home as soon as possible.
We may therefore need to enquire about your home situation, to see if you need any additional support (involvement of the intermediate care team). While on the ward the doctor will talk to you about the operation, the reason why we recommend it and the potential complications and risks of not doing or agreeing to the operation. If you agree with what is told, you would be asked to sign a consent form (giving us permission to go ahead with the operation).
We will also be carrying out assessments of your pressure areas (to prevent development of pressure sores) and nutritional status (to maintain nutrition at optimum levels). You will also receive a welcome card that informs you of the next steps of your treatment and a planned date and time of discharge. If you are fit before this date we will allow you to be discharged earlier. You will also be kept informed of any reasons for delay. Although our wards may care for both male and female patients we endeavour to segregate male and female areas in order to promote privacy and dignity. The nursing and medical team will try and maintain your privacy and dignity at all times. If you have any concerns, please do not hesitate to speak to the nurse in charge.
If you need an operation to repair your broken hip, we would like you to have it within two days of being admitted, unless you have a medical reason for delay.
You will then be taken to the operation theatre, to have your hip repaired
and will receive an anaesthetic. Details of the operation and anaesthetic
(spinal, general or combined) will be explained to you by the Orthopaedic
doctor on duty and the anaesthetist respectively, prior to your operation.
The benefits of the operation are to repair the broken parts which will help
to reduce the pain and allow you to walk again on your leg. As with all surgery there are some risks and complications which you will need to know about.
Pain - this happens with every operation and you will be given tablets to help with the pain.
Bleeding - this can happen with surgery and you may require a blood
transfusion.
Infection in the wound - this usually settles with antibiotics, but may require a further operation.
Blood clots - these can form in your legs initially and may move in the blood stream to your lungs. You will be given medication to help prevent clots.
Chest infection - this can occasionally happen after surgery and you may
require antibiotics and physiotherapy.
Heart attack or a stroke - these can be complications of hip surgery. Both
of these can occasionally cause death.
Damage to the hip nerves - pain, weakness, and numbness may happen,
but normally settles down.
Loosening or dislocation - the metalwork might come loose or your hip
dislocate at a later stage after the surgery. If this happens you may require a further operation.
You will need to be fasted for 8 hours before the operation so as to be able
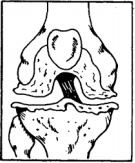
to safely receive an anaesthetic. Depending on where and how complex the break is in your hip, there will be different operations to deal with the fracture. If the neck of the ball part of your hip is broken we would most commonly recommend half a hip replacement (Figure 1).
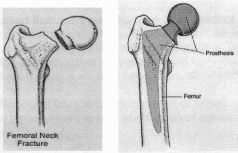
Figure 1 - Thompson’s prosthesis
If the break has left a good blood supply to the ball part of the joint we can fix this with metal screws and a plate (Figure 2).
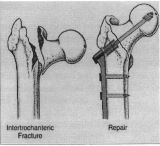
Figure 2 - Dynamic Hip Screw
Following surgery, you will wake up in the recovery ward and then be
transferred to your actual ward, once your blood pressure and temperature have stabilized, and your pain is under control. The doctors and nursing staff will look after your individual care on a daily basis to help your recovery. To reduce the risk of developing clots in your leg veins or lungs we use a once daily injection called Dalteparin, unless there is a contraindication in your case.
The initial part of your stay in the ward, after the operation, is to make you comfortable with the pain. The physiotherapy and nursing team will help you get back on your feet as soon as possible starting from the first day after your operation. They will use a frame initially then as you get better you may be able to use crutches and be able to walk around on your own. It is important that the physiotherapy team thinks that you are safe on yourfeet before we consider getting you home. If you need to practice on the steps or stairs the Physiotherapists will do this with you.
We recognize the fact that many patients have other medical problems,
which need attending to, along with their broken hip. For this reason we
receive input from a dedicated medical team led by an experienced consultant.
This team hopes to look into associated medical conditions that we believe
could have led to or compounded your broken hip.
For this reason we may need to run some special tests, which will be -
• Bone profile (blood tests to check condition of bone)
• Dexa scan (special scan to look at condition of bones - generally done
at a later date)
You may be started on some tablets to strengthen your bones (like Calcium tablets, Vitamin D tablets etc), if we decide it is needed.
Rest is a very important part of recovery and we have specific times when
visitors cannot come on a ward. We have dedicated times for meals to help your recovery and nutritional balance. Please check with the staff on the ward for open visiting times.
We hope you will only need to stay with us for a short period of time and
the ward team will be working with you to make arrangements for your safe discharge back to your home. Some patients may require support in their own home from the Intermediate care team (a team of nurses, carers and therapists who provide skilled care in the community setting) and if so this will be discussed with you. Other patients may require to be considered for an Intermediate care bed in one of the community hospitals eg Longton, Leek, Cheadle, Bradwell or the Haywood. Some patients who have other existing medical problems will require a rehabilitation bed and these are also at Leek, Bucknall and Cheadle hospitals.
You will also have visits from the Occupational therapists, who will help you become independent again and discuss / arrange what equipment you
might need to help you manage. At any point during your stay in this hospital if you have any questions or concerns please do not hesitate to discuss these with the nurse or doctor in charge.
| Visiting Times | Contact Number | |
| WARD 12 | 2 - 4 pm & 6 - 8 pm | 01782 554175 |
| WARD 19 | 2 - 4 pm & 6 - 8 pm | 01782 554172 |
| WARD 24 | 2 - 4 pm & 6 - 8 pm | 01782 554467 |
| HOSPITAL SWITCHBOARD | 01782 715444 | |
| A & E RECEPTION | 01782 554455 | |
| SENIOR CLINICAL NURSE (MATRON) | 01782 554829 |
Contact numbers for any ward other than trauma wards, are available through the hospital switchboard number given above. The staff on these wards are more than happy to answer any queries you may have.
This booklet is designed to provide information about a knee arthroscopy and what to expect before and after this operation. It has been compiled by the Orthopaedic surgeons, nurses, physiotherapists and occupational therapists of North Staffordshire. It is recommended that you read this information before your operation and write down any questions you may have. If you have questions, please feel free to ask a member of the surgical or nursing team. Your surgeon, nursing staff and therapists
will be happy to answer any questions you have regarding your care.
Our staff’s goals are to restore your hips to a painless, functional status and to make your hospital stay as beneficial, informative, and comfortable as possible.
Welcome to the Orthopaedic Outpatients Department at UHNM Orthopaedic and Surgical Unit. When you come for your appointments or to be admitted to hospital for your operation, there is a drop off point and disabled parking spaces outside the main entrance to the Main Clinic Waiting Area. If you have difficulty walking, wheelchairs are available for your use. Please ask at the Reception Desk if you need to use one or if you need a porter to wheel you to the ward. If you are unable to sit for long periods please inform the clinic staff when you arrive so that they can find somewhere for you to lie down. In the Main Waiting Area there is a WRVS coffee bar where you can buy snacks, sandwiches and hot and cold drinks. If you want to have a hot meal while you are waiting there is also a Dining Room in the building within walking distance. Please inform the clinic staff when you arrive if you are diabetic, to help us to avoid
you missing your regular meals. Please let us know as soon as possible if you are unable to attend for an appointment, so that your appointment slot is not wasted.
Arthroscopy is the examination of the inside of the knee with a fibreoptic probe. It has become one of the most frequently used and accurate tools for diagnosis and treatment of knee injures. It is a surgical procedure which is performed as a day case. Through a few small incisions the surgeon can insert the arthroscopy instruments into your knee (keyhole surgery) The arthroscope allows the surgeon to see the entire knee joint and some injuries or disorders such as a cartilage tear can be treated by removal of the loose segment of the cartilage or on occasion a repair of
the cartilage tear. To help you understand your knee injury and the need for the arthroscopy it helps to know a little about the anatomy of a normal knee.
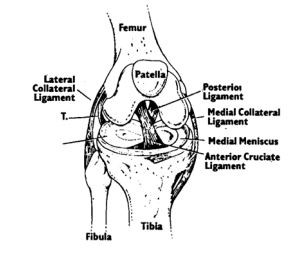
Some of the more common knee problems include meniscus injuries, ligament injuries, degenerative disorders and patella derangements.
Meniscus Injuries
Menisci are the shock absorbing pads of cartilage in your knee. They may tear, split or fray

Ligament Injuries
Ligaments hold the bones together and stabilise your knee. Ligaments may tear completely or partially
Degenerative Disorders
These are caused by changes in the joint surface cartilage. The cartilage may be rough or worn.
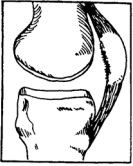
Patella Derangements
The patella is the round bone in the front of your knee. It may be rough
underneath or may not be in the correct position
Your surgeon has recommended you to have an Arthroscopy for you knee. It is however your decision to go ahead with the surgery and the further information in this leaflet may help you decide. If you have any questions that this leaflet does not answer you should ask your surgeon or any member of the health team. Just because your knee hurts it does not mean an arthroscopy is indicated. Your surgeon will consider your symptoms and examine your knee. An ordinary X-ray is usually performed. A MRI scan can be helpful and if normal it is rare that an
arthroscopy will be helpful to you. If there are true mechanical features in your knee i.e. locking, giving way, jamming, it is more likely a problem such as a torn cartilage can be identified and put right.
The main benefit is to find out exactly what your problem is and in most cases treat the problem at the same time. It allows the surgeon to look inside all areas of the joint without a big incision. With keyhole surgery there is a lower risk of complications and a quicker recovery.
Problems inside the knee vary – some may improve with time, some will stay the same and some problems will continue to get worse. You can ask your surgeon whether your particular problem will progress.
The healthcare team will try to make your operation as safe as possible, however some complications can happen.
1. Complications of anaesthesia
This can be discussed with your anaesthetist. These are rare, especially in young people
2. Complications of any operation
• Pain – this happens with any surgery. This will be controlled with medication and it is important that you take this.
• Infection in the wound (< 1 in a 1000)– this usually settles with antibiotics, but may require further surgery.
• Unsightly scarring – this is vary rare as arthroscopy scars are so small, but there may be a small lump for a few weeks.
• Blood clots in the legs (deep vein thrombosis) – these can move through the blood stream into the lungs (pulmonary embolus). You may be given treatment to reduce the risk of blood clotting.
3. Specific complications
• Bleeding in the knee – this may cause more swelling and pain and you may need a further arthroscopy to wash out the knee
• Significant swelling depending on the procedure – this may take several weeks to go down
• Infection in the joint – this is extremely rare, but may require a further wash out of the knee and a course of antibiotics
In a sense one of the most significant lack of benefit is that nothing is found that can be put right and you may continue with your symptoms.
On rare occasions parts of the instruments can break and can usually be retrieved. On rare occasions the operation cannot be completed through the very small puncture wounds where the endoscope is inserted and an open incision may have to be undertaken. We cannot always advise you of this in advance and it is wise to consider this is always a possibility. It does not mean that a major complication has occurred but it may slow your recovery down and you may have a little more pain and need physiotherapy and splintage, or crutches for a slightly longer period.
You will be reviewed before the proposed date of your operation. This allows doctors and nurses to check to see you are medically fit for the anaesthetic and operation. Fresh x-rays and blood tests may be taken.
You will be questioned about your current health and past medical, surgical or medication history. Particularly important things to tell the nurse or doctor about are:
• any heart problems
• asthma or any particular shortness of breath problems
• any bad reactions to a previous anaesthetic
This is an opportunity to tell the nurse of any worries or special needs when you return home after your operation. The operation should not be performed if there are any active infections. If any infections, including a bad cold occurs before your admission, please telephone the Hospital Admissions Officer. You must bring all your current medicines prescribed by your doctor to the Assessment Clinic and on admission to the ward. Smokers must stop prior to surgery to lessen the likelihood of a postoperative chest infection. However, if you are young, fit and healthy, a pre-operative assessment is usually not required.
Most arthroscopic surgery of the knee is undertaken as a day patient procedure under general anaesthetic. Do not eat anything or drink anything after midnight, unless otherwise instructed by the doctor at the hospital.
For day case surgery, personal toiletries may be brought in. Bring your routine medication with you and take routine medicines only as directed by the Anaesthetist or Surgeon. Make arrangements to have a responsible adult available to drive you home after discharge following your day surgery and stay with you overnight. You will not be allowed to leave the hospital alone. You must not drive the same day as a general anaesthetic.
After you are admitted there will be further discussion with the day surgery nursing staff. You may be visited by a physiotherapist who will advise you of simple muscle bracing exercises and use of crutches, however normally this will be done after the surgery. Before the procedure the Anaesthetist will talk to you and assess the most suitable form of anaesthetic, most often a general anaesthetic (being put to sleep). At any
time please ask about the anaesthetic and post-operative analgesia. You may be given a pre-medication to make your wait less anxious. You will be carried to the operating theatre on a trolley or bed.
An arthroscopy can be performed using a variety of anaesthetic techniques lasting for 30-60 minutes depending on the amount of treatment needed. Your anaesthetist will discuss options with you. Under the anaesthetic your surgeon will examine the stability of the knee ligaments and the range of movement. The camera will be inserted via small cuts on the front of
you knee. Your surgeon will examine inside the joint and treat and wash out any loose material. At the end of the procedure any excess fluid is drained from the joint and the incisions are closed with paper or normal stitches and covered with a light dressing.
You will be observed and monitored for a short period in the Recovery Bay area which is close to the theatre. You may have a small drip in a vein which will be removed later in the Ward. Once you are breathing comfortably you will be allowed back in the ward to the Day Unit. You may remain in the Day Unit for an hour or so but this may vary according to the surgical procedure and the type of anaesthesia. Various checks on your blood pressure etc will be taken and your circulation, sensation and comfort will be assessed.
Before discharge you will be asked to stand and walk. You may feel tired and dizzy but this is a normal reaction following anaesthesia. The physio team will assess whether you need crutches to help to walk with and show you how to use these. If you have stairs at home you will practice going up a few steps to make sure you are safe. They will also go through the knee exercises with you. It is not routine to attend outpatient physiotherapy, but if it is felt that you need further treatment then this will
be arranged for you. Analgesics (medication) for pain will be provided for you to take if you have severe pain. You should not drink alcohol when you are taking the medication. As your recovery progresses Paracetamol should be sufficient.
You may feel a little drowsy for 24 or 48 hours and you should have someone at home. You must put as much weight on the operated leg as has been advised by your surgeon or physiotherapist. Keep your bandages clean and dry and do not remove them until you return to the clinic or as instructed by your surgeon. The dressing should not come into contact with water. If you bathe, cover the bandaged leg with a plastic bag, fastening securely beyond the upper edge of the bandage or dressing, with tape.
There may be a small amount of pink or red drainage through the outer surface of the dressing, which is normal. If this increases in amount over a 12 hour period you should report this to the Day Unit or to your General Practitioner. Elevate the operated leg, if possible, in the first 48 hours and an application of an ice pack will also help reduce any pain and swelling. When sleeping a pillow should be used to keep your leg up. Elevation in the first few days is a precaution that can prevent post-operative complications.
Contact the Day Unit nurse or your General Practitioner if the following occurs:
• swelling
• tingling, (pain or numbness in your toes which is not relieved by elevating your foot for a period of one hour)
• foul smell with discharge or drainage from your bandage
• mouth temperature above 38.5ºC or 101 .3ºF
• pain in the operated leg which is not relieved by test, leg elevation or pain medication
The Patient Advice and Liaison Service would be pleased to offer confidential advice and support if you have any concerns. PALS can be contacted on 01782 552814 or Email patient.advice@uhns.nhs.uk
This booklet is designed to provide information about total hip replacement and what to expect before and after this operation. It has been compiled by the Orthopaedic surgeons, nurses, physiotherapists and occupational therapists of UHNM. It is recommended that you read this booklet before your operation and write down any questions
you may have. If you have questions, please feel free to ask a member of the surgical or nursing team. Your surgeon, nursing staff and therapists will be happy to answer any questions you have regarding your care. Our staff’s goals are to restore your hips to a painless, functional status and to make your hospital stay as beneficial, informative, and comfortable as possible.
Welcome to the Orthopaedic Outpatients Department at UHNM Orthopaedic and Surgical Unit. When you come for your appointments or to be admitted to hospital for your operation, there is a drop off point and disabled parking spaces outside the main entrance to the Main Clinic Waiting Area. If you have difficulty walking, wheelchairs are available for your use. Please ask at the Reception Desk if you need to use one or if you need a porter to wheel you to the ward. If you are unable to sit
for long periods please inform the clinic staff when you arrive so that they can find somewhere for you to lie down. In the Main Waiting Area there is a WRVS coffee bar where you can buy snacks, sandwiches and hot and cold drinks. If you want to have a hot meal while you are waiting there is also a Dining Room in the building within walking distance. Please inform the clinic staff when you arrive if you are diabetic, to help us to avoid you missing your regular meals. Please let us know as soon as possible if you are unable to attend for an appointment, so that your appointment slot is not wasted.
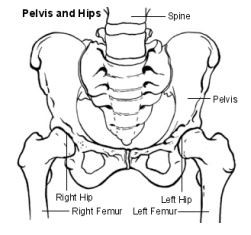
Total hip replacement is a surgical procedure for replacing the hip joint. This joint is composed of two parts – the hip socket (acetabulum, a cup-shaped depression in the pelvis) and the ‘ball’ or head of the thigh bone (femur). During the surgical procedure, these two parts of the hip joint are removed and replaced with smooth artificial surfaces. The artificial socket is made of high-density plastic, while the artificial ball with its stem is made of a strong stainless metal. These artificial pieces are implanted in healthy portions of the pelvis and thigh bone and affixed with a bone cement (methyl methacrylate) or special coatings that encourage bone in growth.

Total hip replacements are usually performed for severe arthritic conditions, of which there are many. However, we sometimes perform the operation after other problems such as hip fractures or avascular necrosis (a condition in which the blood supply to the centre of the hip ball fails). Most of the patients who have artificial hips are over 55 years of age, but we occasionally perform the operation in younger persons in particular circumstances. The circumstances vary somewhat, but generally patients are considered for hip replacements if:
• They have significant pain during the day or night.
• The pain is severe enough to restrict not only work and recreation, but also the ordinary activities of daily living.
• The pain is not relieved by arthritis (anti-inflammatory) medicine, the use of a stick, and is restricting activities.
• They have significant stiffness of the hip.
• X-rays show advanced arthritis, or one of the other problems mentioned.
• They weigh less than 180 to 190 pounds (Approx. 80.45kg).
An artificial hip replacement is not a normal hip, nor is it as good as a normal hip. The operation will, however, provide complete, or nearly complete, pain relief in 90% to 95% of patients for up to 10 years. It will allow those patients who get pain relief to carry out the normal activities of daily living. It will not, however, allow patients to return to active sports or heavy labour. Activities must be avoided which overload the artificial hip. Most patients (70-80%) with stiff hips before surgery will regain near-normal motion, and nearly all (85-90%) have improved motion.
The major long-term problem is loosening. This occurs either because the cement crumbles up (as old mortar in a brick building) or because the bone melts away (resorbs) from the cement. By 10 years 15% of all artificial hips will look loose on x-ray. Somewhat less than half of these (about 5% to 10% of all artificial hips) will be painful and require re-operation. By ten years probably 5% to 10% will require re-operation.
Loosening is in part related to how heavy you are and how active you are. It is for this reason we try to avoid operating on very overweight patients or young, active patients. (In patients under 50 years, a greater proportion of hips loosen). Loose painful artificial hips can usually, but not always, be replaced. The results of a second operation are not as good as the first, and the risks of complications are higher.
A new hip has been developed that does not require cement. This hip has the potential to allow bone to grow into it, and therefore may last longer than the cemented hip. This is a particularly important consideration for the younger patient. Another possible advantage of this new hip is a
lower infection risk and possible easier revision surgery, should this be necessary. The complications that can occur with the new non-cemented hip are similar to those which may occur with the standard cemented prostheses. Your surgeon will discuss the choices in your case. Some patients with cementless hips have slight aching.
Total hip replacement is a major operation and there can be complications. However the effect of most complications is simply that the patient stays in hospital a little longer. The complications specific to a total hip replacement fall into three categories: complications of anaesthesia, complications of any operation and complications specific to having a hip replacement.
Anaesthetic risk
There is a very small risk of a heart attack following hip replacement and also a risk of stroke and chest infections. Your anaesthetist will see you before your operation to discuss the risks and the anaesthetic choices available. The choices are general anaesthetic, spinal anaesthetic or a combination of these. Your anaesthetist will be able to advise you of which technique might be more suitable for you, taking into account your general health. The most common complications are not directly related to the hip and do not usually affect the results of the operation.
These include:
• Deep vein thrombosis or DVT is a blood clot in the veins of your leg – 10-20% of patients.
Occasionally the clot can dislodge and travel to the lungs (pulmonary embolus). The risk of a fatal embolism is very small. To help avoid thrombosis the physiotherapists and nurses will get you moving around as soon as possible, usually on the day after your surgery. You will be
given blood-thinning medication to prevent blood clots forming and you may also be fitted with special elastic anti-embolism stockings (TED stockings) on admission. These help increase the blood flow in your legs and they are usually worn for six weeks after surgery.
• Difficulty passing urine may occur – 20% patients. This might mean you needing a catheter (small tube) to drain your bladder for a day or two.
• Pain, which happens with every operation. See the section on pain management for information about ways in which the team will try to reduce your pain
• Temporary nausea and vomiting – 10% of patients.
• Blood clots in the lung 1-2% of patients.
• Infection in the surgical wound can be a complication of any operation. Usually these clear up quickly with antibiotics.
Complications that affect the hip are less common, but in these cases, the operation may not be as successful:
• Difference in leg length – 10% of patients. The surgeon will make every effort to maintain the length of the leg, but there is no guarantee
• Stiffness – 10% of patients
• Persistent hip pain – 5% of patients
• Dislocation of hip (ball pops out of socket) – 2% of patients
• Infection in hip – 1% of patients Infection can result in loosening and failure of the replacement over a period of a few months. One or more further operations will usually be needed to control the infection (risk 1 in 50). Some infections like MRSA (Methicillin Resistant Staphylococcus Aureus) are resistant to common antibiotics and therefore are more difficult to treat. At the Pre-operative Assessment we screen for MRSA by taking swabs from the nose and perineum of all patients coming in for joint replacement surgery
• Haematoma (swelling due to bleeding) in thigh – 1% of patients.
• Nerve injury – rare. The sciatic nerve is at the back of the hip and can be damaged during surgery. This may lead to numbness or weakness in the leg.
• Blood vessel and bone damage – rare. There can also be minor damage to local blood vessels or the bone itself.
Other complications may occur, but these happen in less than ¼ percent of patients (one patient in four hundred): death, fractures, etc. A few of the complications, such as infection, dislocation, and haematoma, may require re-operation. Infected artificial hips sometimes have to be removed, leaving a short (by one to three inches) somewhat weak leg, but one that is usually reasonably comfortable and one on which you can walk with the aid of a stick or crutches. It must be emphasized that these are rare problems and most patients are pleased with the results of their operation.
• Antibiotics are administered to counter infections
• Anti-clotting agents are commonly used unless there is a contra indication (stomach ulcers)
• Special stockings and early mobilisation to minimise the likelihood of blood clots (venous thrombosis).
It is important that you are fit for your operation as you will make a quicker recovery. If you smoke, try to cut down or quit, ideally 8 weeks or more before your operation. Smoking changes blood flow patterns, delays healing and slows recovery. Even stopping for 24 hours before the operation is beneficial. If you want to stop smoking ask for information about the Smoking Cessation Nurse or talk to your General Practitioner or Practice Nurse.
Keep your weight down. Being very overweight (i.e. a Body Mass Index of greater than 30) can significantly increase the risk of complications from surgery and anaesthesia, make the operation more difficult and reduce the life of your hip replacement. The assessment nurse will weigh you and
measure your height and give you some advice. You may find it helpful to talk to your General Practitioner or Practice Nurse. If you are seriously overweight your consultant may delay surgery until you have lost some weight.
Have a dental check if you have not done so in the last six months. It is important that any dental infections are dealt with before joint replacement surgery to prevent infection in your new hip. If infection is suspected your operation will be postponed.
Practice sleeping on your back- you will not be allowed to lie on your side for approximately six weeks following surgery.
Keep yourself fit - Being as fit as possible before the operation will speed recovery and reduce the risk of complications. It is worth trying to walk a short distance each day as pain permits, or take up gentle exercise such as swimming to improve your level of fitness and mobility. Activities which
improve upper limb strength will improve your ability to use walking aids after the operation.
Getting the full benefit from hip replacement surgery can take a few months and during this time a full range of movement may be difficult. As a consequence many people find they are limited in their ability to do normal activities such as bathing, shopping, laundry, cooking and housework. Help from others may be needed. It is important to plan ahead and think about the support you will need when you go home, usually at around three days after surgery.
Here are some suggestions to start thinking about:
♦ Arrange for someone to take you home from the hospital. The average stay in hospital is about 4- 5 days. You will not be allowed to drive for at least six weeks after your operation, until you have been reviewed in clinic. Before driving it is important to notify your car insurance company.
♦ If you are caring for someone else you will need to make alternative arrangements for their care (respite, home care, help from friends or family, your GP maybe of help in making these arrangements).
♦ Is anyone available to help you when you come out of hospital? It is better if someone can be with you for the first week or two following discharge to help with things like cooking and personal care, if only for part of the day, whilst you gain you’re confidence.
♦ It is a good idea to prepare and freeze some meals in advance or arrange for relatives and friends to bring meals and assist with shopping.
♦ Organise your kitchen to avoid excessive lifting and bending. The Occupational Therapist can advise you on the use of equipment to assist you in the kitchen.
♦ Remove any rugs or mats that could cause you to trip. Securely fasten any electric wires and ensure a safe passage throughout your home.
♦ Do not fly or go on long journeys before 6 weeks as this increases your risk of DVT or PE
The Occupational Therapist (OT) will assess your requirements and order any appropriate equipment to help you once you are at home. You will be asked to provide information about your home environment and how you are coping at home prior to your admission. The OT will discuss and show
you how to carry out activities of daily living safely, without excessive bending. They will also discuss managing everyday activities safely after hip surgery. You will require a suitable armchair. The OT will advise you on the height of the chair. It must not be too low, soft or deep. You should be able to get out of the chair easily without bending your hip at more than a right angle. Swivel office chairs are not recommended. Depending on the height of your toilet seat you may require a raised toilet seat for at least 6 weeks. Your bed also needs to be of a suitable height. It is important to remember the above when visiting other places e.g friends, church, restaurant.
You will generally be called up to the hospital before the proposed date of your operation. This allows doctors and nurses to check to see you are medically fit for the anaesthetic and operation. Fresh x-rays and blood tests may be taken. You will be questioned about your current health and past medical, surgical or medication history.
Particularly important things to tell the nurse or doctor about are:
• Myocardial infarcts (heart attack)
• Asthma
• Any particular shortness of breath problems
• Allergies
• Any bad reactions to a previous anaesthetic
This is an opportunity to tell the nurse of any worries or special needs when you return home after your operation. The operation cannot be performed if there are any active infections. If any infections, including a bad cold occur after your assessment but before your admission, please telephone the Admissions Officer or your Surgeon’s Secretary.
• You must bring all your current medicines prescribed by your doctor to the Assessment Clinic and on admission to the ward. If you take medicine for high blood pressure it would be helpful to bring some recent blood pressure readings. If you are diabetic please bring a record of your blood ugar readings. If you are on Warfarin please bring your yellow book.
• Smokers must stop prior to surgery to lessen the likelihood of a post operative chest infection.
• You will be asked at this pre-operative assessment to sign to give your consent for us to perform the operation.
• We often start iron tablets to build up your bodies iron stores ready for surgery. We will give you a bottle of skin cleansing liquid to use at home on the night before you come into hospital, which reduces your chance of wound infection
• This is an opportunity to ask further questions if you are unsure of anything.
Your operation date will usually be given to you. If you are unable to keep your appointment for admission or for preoperative assessment please inform us as soon as possible using the contact numbers at the back of this booklet. Late cancellations waste operating time and lengthen the waiting list.
Usually you will be admitted to the ward on the day of your operation.
Please only bring on admission what you will need for the first couple of days such as medication, toiletries, nightwear, glasses etc. due to limited storage space. We suggest that you put other items on one side at home for your family / friends to bring in for you later.
Before the operation the anaesthetist will talk to you and assess the most suitable form of anaesthetic. Your anaesthetist may recommend a pre-medication to be given some hours before surgery. This is an injection or tablet that will make your wait less anxious. The Nursing Staff will discuss with you your general needs and what to expect before and after your operation. A period of fasting i.e. nothing to eat or drink for some hours before surgery is necessary as this will reduce the risk of vomiting. This is another opportunity to ask any questions you may have. Any extra help you may require when you are discharged home should be mentioned. It is best to prepare well ahead!
The Nursing Staff will ensure you have a complete all over shower (as your physical limitations allow) using an antiseptic soap. The side of the operation must be marked and/or a label affixed to you detailing the procedure to be undertaken. These are all safeguards. You will be carried on a trolley or bed to the theatre.
After your operation you will be observed and monitored until you have recovered from the effects of the anaesthetic. There will be an intravenous infusion (drip in your arm) and drain tubes coming out of your thigh for 24 hours of so. These prevent excess post-operative blood collections. They are not painful and are easily removed by the nursing staff at about 24 hours with only slight discomfort. Nausea and sickness are quite common side-effects of the general anaesthetic and painkillers. If you feel sick please let the nursing staff know as anti-sickness medicine is available to help reduce these symptoms and being unable to eat may slow down your recovery. You will be able to eat as soon as you feel like it. You will be given oxygen through a mask for a few hours.
Some discomfort or pain after surgery is normal. The nursing staff will assist you to control any pain through injections or tablets.
Your anaesthetist or pain nurse will discuss the best method of controlling your pain with you. There is a form of pain relief available called a PCA (Patient Controlled Analgesia). This means you will have a pump, which you control yourself to administer small doses of pain-killer by pressing a
button on the handset whenever you need more pain relief. It is very safe and you will be closely monitored by nursing staff. Another form of pain relief is an epidural. The anaesthetist inserts a thin hollow needle into the
epidural space, just outside the outer covering of the spinal cord in the lower back. A small plastic tube is then introduced through the needle and left in position when the needle is removed. The tube is used to introduce local anaesthetic and pain killing medication. An epidural provides pain relief for as long as it remains in place, usually overnight. It may cause some temporary numbness and weakness in the legs, which wears off after three or four hours.
The Nursing Staff will assess you regularly to find out how comfortable you are. Suffering from pain can slow down recovery, so please tell the Nursing Staff if you are in pain at any time. While the pain may be acceptable when you are resting, it will increase when you move, and it is important to change position regularly and do exercises 5-6 times a day following the operation, so it is important to take pain relief regularly. We will be happy to help you in any way to make your stay as comfortable as possible.
You will probably be nursed on your back initially with your operated limb on a pillow or support. Sometimes a foam wedge or skin traction is used – the nurse or the doctor will explain the need for this.
On the first day after your operation the physiotherapists will see you. They will show you some leg exercises to help with the circulation. If you feel well enough they will help you to sit onto the side of the bed and stand using a frame. You must follow the exercises given to you, contracting your calf muscles and moving your toes. If you feel soreness of your heel or tail bone (sacral area) you must tell the nurses. Various blood tests and x-rays will be taken and you may have a blood transfusion. On the second day after surgery the physiotherapists will help you get out of bed again and try a small walk with a frame. Then on a daily basis you will practice your walking and as soon as you are able start using elbow crutches. If you have stairs at home the physios will practice this with you to make sure you are safe to go home. The occupational therapists will also see you to see if you require any equipment assistance for when you go home.
You will be shown the safe way to:
• Sit and stand up from a chair
• Get on and off the bed
• Go to the toilet
• Complete washing and dressing
• Prepare meals and a drink
You must not lean forward or flex your hip up or turn when sitting, cross you legs or attempt to pick anything up from the floor. These simple rules are to minimise the likelihood of the new hip dislocating (‘ball coming out of socket’) (see later for more detailed advise on mobilisation and selfcare).
Upon discharge from the hospital, you probably will have achieved some degree of independence in walking with crutches or a walker, climbing a few stairs, and getting into and out of bed and on and off chairs. Nevertheless, you will need some help at home to assist you for a week or so. Get family to help with lower half garments or seek help from the Occupational Therapist or Physiotherapist for dressing gadgets. You may need to wear elastic (TED) stockings for six weeks after your operation.
The Community Intermediate Care Team is a team of Qualified Nurses, Health Care Support Workers, Social Services Staff, Rehabilitation Support Workers and Therapists who can support your discharge home following your hip replacement. It is our normal level of care to discharge you back to your own home as soon as it is reasonable to do so, usually 3 days after surgery and to provide you with the support you need at home. A member of the team will visit your home on the day after your discharge from hospital between 9am and 5pm to offer support and continue with treatment in your own home. They will provide the most appropriate care package for you, tailored to your individual needs. Not every patient will require therapy input.
The team also works very closely with other colleagues in the community, such as District Nursing teams and Social Services and will liaise with these services if you require ongoing care and support in your own home.
It is important to continue with your exercises. The success of the operation has a lot to do with how well you do your exercises and strengthen your muscles. This part of your recovery is very much down to you.If excess muscle aching occurs, cut back on your exercises but do not stop. Wound stitches or staples are removed on about the fourteenth day after surgery.The Community Intermediate Care Team will arrange for a District Nurse to visit you in your own home.
Upon returning home, you should be alert for certain warning signs. If you notice any swelling, increased pain, drainage from the incision site, redness around the incision, or fever, you should report this immediately to your doctor.
Whilst on bed rest, general exercises are very helpful.
These consist of:
1. Deep breathing and coughing to prevent post-operative chest infection following the anaesthetic.
2. Wiggling your toes.
3. Moving your feet up and down and tightening your calf muscles.
4. Tightening your thigh muscles.
5. Squeezing your buttocks together.
6. Bending and straightening your operated leg. To increase range of movement, you can help by using your hands.
7. Lying flat, take your operated leg out to the side (abduction) and back to the middle.
Get in and out of bed on the OPERATED side wherever it is possible. If your bed at home cannot be moved, take care not to let the leg roll in, as you get in and out. Sit down on the edge of the bed, push yourself further onto the bed and then keeping your legs TOGETHER and straight swing them onto the bed. Reverse the procedure when getting out of bed. DO NOT bend over at the hip.
You will commence walking using a Zimmer frame or elbow crutches.
The sequence is always:
1. Walking aid moved first
2. when operated leg, and
3. finally, un-operated leg.
You can turn round either way (although your surgeon may advise you to turn away from your operated hip) but you must prevent pivoting or twisting your hip. Therefore, you must pick up your feet at each step making sure that the operated leg is not rotated too far in or out. As your walking and confidence increase, you will usually progress to using two sticks.
The sequence will be:
1. Right stick, left leg
2. Left stick, right leg
It is advisable to sit in a high firm-backed chair with arms. You must feel for the chair with the back of your legs (a) and for the arms of the chair with your hands (b), sit down with your operated leg placed out in front of you taking the weight of your good leg (c and d).
You will be taught how to do this by the Physiotherapist or Occupational Therapist. The same procedure is used for the toilet but with the aid of a raised toilet seat, if necessary.
Often your operated leg will be supported on a stool to prevent ankle swelling. Do not sit too long – if there is any ankle swelling it is better to rest on the bed rather than to sit. Always avoid low sofas etc… Do not turn or trust your body when standing on your operated let or sitting.
It is useful to use the opposite hand to the operated leg when putting on socks, stockings, etc. If you live alone the Occupational Therapist will assess you for dressing gadgets such a stocking aid or long-handled shoe horn.
To retrieve fallen objects from the ground place your operated leg behind you and balance with your hand on a firm surface or stick bending forward from the waist and your good leg. If you live alone the Occupational Therapist will provide a “helping hand” to enable you to pick up items from the floor.
It is not advisable to get into a bath for 6 weeks. If you have a walk-in shower, this is ideal. If however there is a high step up to the shower you may need a block/small stool to help you get in and out. Bath seats and boards can be obtained from certain shops.
You will be taught how to negotiate stairs by the Physiotherapist. Banisters should be used with your free hand when possible:
Remember
1. Good leg leads up.
2. Operated leg leads down.
3. Stick stays with the operated leg.
Therefore, going upstairs:
1. Un-operated leg first.
2. Followed by operated leg.
And going down stairs:
1. Stick.
2. operated leg
3. and finally, un-operated leg
Getting in
1. Slide passenger seat back to give you as much leg room as possible.
2. Recline passenger seat to give you more room.
3. Put a cushion/pillow on the seat to raise it up a little higher.
4. Put a large plastic bag on the seat to help you ‘move’ easily (reduces friction) or wear a ‘shell’ suit.
5. Sit down bottom first using car door edge to steady you.
6. Grip both legs together or hook the foot of the un-operated leg under the operated leg or have someone to help you lift the leg into the car.
Turn 90° so both legs are on the ground outside the car. Use the car door edge to help you stand. Then have someone pass the crutches to you. Surgeons generally recommend that patients do not drive their car for a minimum of 6 weeks after the operation. You may be wise to alert your insurance company.
If you have ACUTE pain with swelling in the calf muscle, or swelling or wound redness at home, call your General Practitioner.
AVOID TWISTING THE OPERATED LEG WHEN WALKING, e.g. WHEN TURNING AROUND.
It depends on your job. It is possible to return at 8-10 weeks for those that do not perform manual work.
If at any time (even years after your surgery) you develop a bacterial infection such as sore throat or significant chest, urinary infection or cellulitis (redness and swelling of the limb) you should inform your General Practitioner of your hip replacement. Antibiotics should be administered promptly to prevent the occasional complication of distant infection localizing in the hip area. This also applies if you have any teeth extracted.
DO:
- Carry on with the exercises as instructed by your physiotherapist
- Take regular short walks
- Keep walking with your walking aids until 4 to 6 weeks after your operation. You will then progress to 1 walking stick held in the opposite hand to your new hip.
- Stand and sit as shown in hospital – operated leg in front, push on the arms of the chair, bed mattress or toilet seat frame
- Avoid pressure on the wound until it has fully healed and keep the wound dry until the skin has fully healed
- Avoid picking up objects from the floor or reaching down, unless you have been shown the correct method by the Therapist. Do not reach for objects when sitting, use a ‘helping hand’ for small objects. I f you live alone you will be given one.
- Go to your GP if you have an unusual pain, temperature, notice a discharge from your wound or any pain or swelling in your calves
- Please return any sticks or equipment when you have finished with them
- Ensure you take regular pain-killers for as long as you need to
- Eat a balanced diet with plenty of fresh fruit and vegetables
Until reviewed by your surgeon or a member of their team DO NOT:
- Twist the operated leg in or out whilst sitting or standing for at least 3 months
- Cross your legs, knees or ankles for at least 3 months
- Sit on low chairs, stools or toilets
- Drive a vehicle until advised it is safe to do so. Usually this is after 6 weeks if you can sit comfortably in your car and perform an emergency stop safely.
- Do any heavy lifting, housework or gardening
- Discard any walking aids until advised to do so
- Do too much too soon – gradually increase your activities as able.
- Return to work or sporting activities until advised to do so
Once you return home (in the first few weeks) if you have any questions or concerns that regarding your hip replacement call the Pre-operation Orthopaedic Clinic on (01782) 553216 if your operation was performed at the UHNM. Your General Practitioner can always advise on general matters and will tell you how to get further advice with the urgency the situation demands.
Ward 121 01782 553748
Ward 124 01782 552700
The Patient Advice and Liaison Service would be pleased to offer confidential advice and support if you have any concerns. PALS can be contacted on 01782 552814 or Email patientadvice.uhnm@nhs.net
This booklet is designed to provide information about total knee replacement and what to expect before and after this operation. It has been compiled by the Orthopaedic surgeons, nurses, physiotherapists and occupational therapists of UHNM. It is recommended that you read this information before your operation and write down any questions you may have. If you have questions, please feel free to ask a member of the surgical or nursing team. Your surgeon, nursing staff and therapists will be happy to answer any questions you have regarding your care. Our staff’s goals are to restore your hips to a painless, functional status and to make your hospital stay as beneficial, informative, and comfortable as possible.
Welcome to the Orthopaedic Outpatients Department at the UHNM Orthopaedic and Surgical Unit. When you come for your appointments or to be admitted to hospital for your operation, there is a drop off point and disabled parking spaces outside the main entrance to the Main Clinic Waiting Area. If you have difficulty walking, wheelchairs are available for your use. Please ask at the Reception Desk if you need to use one or if you need a porter to wheel you to the ward. If you are unable to sit for long periods please inform the clinic staff when you arrive so that they can find somewhere for you to lie down.
In the Main Waiting Area there is a coffee bar where you can buy snacks, sandwiches and hot and cold drinks. If you want to have a hot meal while you are waiting there is also a Dining Room in the building within walking distance. Please inform the clinic staff when you arrive if you are diabetic, to help us to avoid you missing your regular meals. Please let us know as soon as possible if you are unable to attend for an appointment, so that your appointment slot is not wasted.
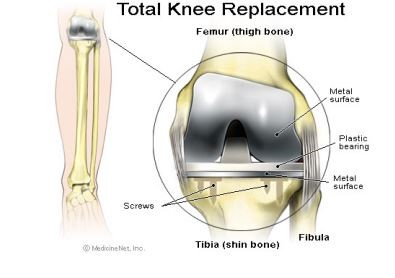
Total knee replacement is a surgical procedure for replacing the knee joint. This joint is composed of three parts – lower end of the femur (thigh bone), the upper end of the tibia (shin bone) and patella (knee cap). During the surgical procedure, diseased surfaces of the knee joint are removed and replaced with smooth artificial surfaces. The femoral surface is of curved polished metal. The tibia is usually metal covered with high density plastic and the knee cap is plastic. These artificial pieces are attached to the bones with a bone cement (methyl methacrylate) or special coatings that encourage bone ingrowth.
Total knee replacements are usually performed for severed arthritic conditions, of which there are many. However, we sometimes perform the operation after other problems such as the late effects of knee fractures or aseptic necrosis (a condition in which the bone of the knee dies). Most of the patients who have artificial knees are over 55 years of age, but we occasionally perform the operation in younger persons in particular circumstances.
The circumstances vary somewhat, but generally patients are considered for knee replacements if:
• They have significant pain during the day or night.
• The pain is severe enough to restrict not only work and recreation, but also the ordinary activities of daily living, especially walking.
• The pain is not relieved by arthritis (anti-inflammatory) medicine, the use of a stick, and restricting activities.
• They have significant stiffness of the knee.
• X-rays show advanced arthritis, or one of the other problems mentioned.
• They weigh less than 180 to 190 pounds (kilo equivalent).
What can be expected of a total knee replacement?
An artificial knee replacement is not a normal knee, nor is it a good as a normal knee. The operation will, however, provide complete, or nearly complete, pain relief in 90 to 95% of patients for up to 10 Years. It will allow those patients who get pain relief to carry out the normal activities of daily living. It will not, however, allow patients to return to active sports or heavy labour. Activities must be avoided which overload the artificial knee. Most patients (70-80%) with stiff knees before surgery will regain useful motion, but 5-10% remain somewhat stiff although pain is usually relieved.
The major long-term problem is loosening. This occurs either because the cement crumbles up (as old mortar in a brick building) or because the bone melts away (resorbs) from the cement. By 10 years 15% of all artificial knees will look loose on x-ray. Somewhat less than half of these (about 5% to 10% of all artificial knees) will be painful and require re-operation. Loosening is in part related to how heavy you are and how active you are. It is for this reason we try to avoid operating on very overweight patients or young, active patients. (In patients under 50 years, a greater proportion of knees loosen). Loose, painful artificial knees can usually, but not always, be replaced. The results of a second operation are not as good as the first, and the risks of complications are higher. Cementless total knee replacement A new knee has been developed that does not require cement. This knee has the potential to allow bone to grow into it, and therefore may last longer than the cemented knee. This is a particularly important consideration for the younger patient. Another possible advantage of this new knee is a lower infection risk and possible easier revision surgery, should this be necessary. The complications that can occur with the new non-cemented knee are similar to those which may occur with the standard cemented prostheses. Your surgeon will discuss the choices in your case.
Total knee replacement is a major operation and there can be complications. However the effect of most complications is simply that the patient stays in hospital a little longer. The complications specific to a total hip replacement fall into three categories: complications of anaesthesia, complications of any operation and complications specific to having a knee replacement. Anaesthetic risk. There is a very small risk of a heart attack following knee replacement and also a risk of stroke and chest infections. Your anaesthetist will see you before your operation to discuss the risks and the anaesthetic choices available. The choices are general anaesthetic, spinal anaesthetic or a combination of these. Your anaesthetist will be able to advise you of which technique might be more suitable for you, taking into account your general health. The most common complications are not directly related to the knee and do not usually affect the results of the operation.
These include:
• Deep vein thrombosis or DVT is a blood clot in the veins of your leg – 10-20% of patients.
Occasionally the clot can dislodge and travel to the lungs (pulmonary embolus). The risk of a fatal embolism is very small. To help avoid thrombosis the physiotherapists and nurses will get you moving around as soon as possible, usually on the day after your surgery. You will be
given blood-thinning medication to prevent blood clots forming and you may also be fitted with special elastic anti-embolism stockings (TED stockings) on admission. These help increase the blood flow in your legs and they are usually worn for six weeks after surgery.
• Difficulty passing urine may occur – 20% patients. This might mean you needing a catheter (small tube) to drain your bladder for a day or two.
• Pain, which happens with every operation. See the section on pain management for information about ways in which the team will try to reduce your pain.
• Temporary nausea and vomiting – 10% of patients.
• Blood clots in the lung 1-2% of patients.
• Infection in the surgical wound can be a complication of any operation. Usually these clear up quickly with antibiotics.
Complications that affect the knee are less common, but in these cases, the operation may not be as successful:
• Stiffness in knee – 10% of patients
• Persistent knee pain – 5% of patients
• Dislocation of patella (knee cap) – 5% of patients – usually 5-10 years post surgery
• Infection in knee joint – 2% of patients Infection can result in loosening and failure of the replacement over a period of a few months. One or more further operations will usually be needed to control the infection (risk 1 in 50). Some infections like MRSA (Methicillin Resistant Staphylococcus Aureus) are resistant to common antibiotics and therefore are more difficult to treat. At the Pre-operative Assessment we screen for MRSA by taking swabs from the nose and perineum of all patients coming in for joint replacement surgery
• Haematoma (swelling due to bleeding) in thigh – 5% of patients.
Other complications may occur, but these happen in less than ¼ percent of patients (one patient in four hundred): death, fractures, nerve injury. A few of the complications, such as infection, dislocation, and haematoma, may require re-operation. Infected artificial knees sometimes have to
be removed, leaving a short (by one to three inches) somewhat weak leg, but one that is usually reasonably comfortable and one on which you can walk with the aid of a stick or crutches. It must be emphasized that these are rare problems and most patients are pleased with the results of their operation.
• Antibiotics are administered to counter infections
• Anti-clotting agents are commonly used unless there is a contra indication (stomach ulcers)
• Special stockings and early mobilisation to minimise the likelihood of blood clots (venous thrombosis).
It is important that you are fit for your operation as you will make a quicker recovery.
If you smoke, try to cut down or quit, ideally 8 weeks or more before your operation. Smoking changes blood flow patterns, delays healing and slows recovery. Even stopping for 24 hours before the operation is beneficial. If you want to stop smoking ask for information about the Smoking Cessation Nurse or talk to your General Practitioner or Practice Nurse.
Keep your weight down. Being very overweight (i.e. a Body Mass Index of greater than 30) can significantly increase the risk of complications from surgery and anaesthesia, make the operation more difficult and reduce the life of your knee replacement. The assessment nurse will weigh you and measure your height and give you some advice. You may find it helpful to talk to your General Practitioner or Practice Nurse. If you are seriously overweight your consultant may delay surgery until you have lost some weight.
Have a dental check if you have not done so in the last six months. It is important that any dental infections are dealt with before joint replacement surgery to prevent infection in your new hip. If infection is suspected your operation will be postponed.
Practice sleeping on your back- you may find it uncomfortable to lie on your side for approximately six weeks following surgery. If you want to you can put a pillow between your knees.
Keep yourself fit - Being as fit as possible before the operation will speed recovery and reduce the risk of complications. It is worth trying to walk a short distance each day as pain permits, or take up gentle exercise such as swimming to improve your level of fitness and mobility. Activities which improve upper limb strength will improve your ability to use walking aids after the operation.
Getting the full benefit from knee replacement surgery can take a few months and during this time a full range of movement may be difficult. As a consequence many people find they are limited in their ability to do normal activities such as bathing, shopping, laundry, cooking and housework. Help from others may be needed. It is important to plan ahead and think about the support you will need when you go home, usually at around three days after surgery.
Here are some suggestions to start thinking about:
♦ Arrange for someone to take you home from the hospital. The average stay in hospital is about 4-5 days. You will not be allowed to drive for at least six weeks after your operation, until you have been reviewed in clinic. Before driving it is important to notify your car insurance company.
♦ If you are caring for someone else you will need to make alternative arrangements for their care (respite, home care, help from friends or family, your GP maybe of help in making these arrangements).
♦ Is anyone available to help you when you come out of hospital? It is better if someone can be with you for the first week or two following discharge to help with things like cooking and personal care, if only for part of the day, whilst you gain you’re confidence.
♦ It is a good idea to prepare and freeze some meals in advance or arrange for relatives and friends to bring meals and assist with shopping.
♦ Organise your kitchen to avoid excessive lifting and bending. The Occupational Therapist can advise you on the use of equipment to assist you in the kitchen.
♦ Remove any rugs or mats that could cause you to trip. Securely fasten any electric wires and ensure a safe passage throughout your home.
♦ Do not fly or go on long journeys before 6 weeks as this increases your risk of DVT or PE
The Occupational Therapist (OT) will assess your requirements and order any appropriate equipment to help you once you are at home. You will be asked to provide information about your home environment and how you are coping at home prior to your admission. The OT will discuss and show you how to carry out activities of daily living safely, without excessive bending. They will also discuss managing everyday activities safely after knee surgery. You will require a suitable armchair. The OT will advise you on the height of the chair. It must not be too low, soft or deep. Initially the limited movement in your knee may make it difficult to get out of a low chair. Swivel office chairs are not recommended. Depending on the height of your toilet seat you may require a raised toilet seat for at least 6 weeks. Your bed also needs to be of a suitable height. It is important to remember the above when visiting other places e.g friends, church, restaurant.
You will generally be called up to the hospital before the proposed date of your operation. This allows doctors and nurses to check to see you are medically fit for the anaesthetic and operation. Fresh x-rays and blood tests may be taken. You will be questioned about your current health and past medical, surgical or medication history. Particularly important things to tell the nurse or doctor about are:
• Myocardial infarcts (heart attack)
• Asthma
• Any particular shortness of breath problems
• Allergies
• Any bad reactions to a previous anaesthetic
This is an opportunity to tell the nurse of any worries or special needs when you return home after your operation. The operation cannot be performed if there are any active infections. If any infections, including a bad cold occur after your assessment but before your admission, please telephone the Admissions Officer or your Surgeon’s Secretary.
• You must bring all your current medicines prescribed by your doctor to the Assessment Clinic and on admission to the ward. If you take medicine for high blood pressure it would be helpful to bring some recent blood pressure readings. If you are diabetic please bring a record of your blood sugar readings. If you are on Warfarin please bring your yellow book.
• Smokers must stop prior to surgery to lessen the likelihood of a post operative chest infection.
• You will be asked at this pre-operative assessment to sign to give your consent for us to perform the operation.
• We often start iron tablets to build up your bodies iron stores ready for surgery. We will give you a bottle of skin cleansing liquid to use at home on the night before you come into hospital, which reduces your chance of wound infection
• This is an opportunity to ask further questions if you are unsure of anything. Your operation date will usually be given to you. If you are unable to keep your appointment for admission or for preoperative assessment please inform us as soon as possible.
Late cancellations waste operating time and lengthen the waiting list. Your admission to hospital Usually you will be admitted to the ward on the day of your operation. Please only bring on admission what you will need for the first couple of days such as medication, toiletries, nightwear, glasses etc. due to limited storage space
We suggest that you put other items on one side at home for your family / friends to bring in for you later. Please bring some sensible loose fitting shoes to make you more safe with your walking practice
Before the operation the anaesthetist will talk to you and assess the most suitable form of anaesthetic. Your anaesthetist may recommend a pre-medication to be given some hours before surgery. This is an injection or tablet that will make your wait less anxious. The Nursing Staff will discuss with you your general needs and what to expect before and after your operation. A period of fasting i.e. nothing to eat or drink for some hours before surgery is necessary as this will reduce the risk of vomiting. This is another opportunity to ask any questions you may have. Any extra help you may require when you are discharged home should be mentioned. It is best to prepare well ahead!
The Nursing Staff will ensure you have a complete all over shower (as your physical limitations allow) using an antiseptic soap. The side of the operation must be marked and/or a label affixed to you detailing the procedure to be undertaken. These are all safeguards. You will be carried on a trolley or bed to the theatre.
After your operation you will be observed and monitored until you have recovered from the effects of the anaesthetic. There will be an intravenous infusion (drip in your arm) and drain tubes coming out of your thigh for 24 hours of so. These prevent excess post-operative blood collections. They are not painful and are easily removed by the nursing staff at about 24 hours with only slight discomfort. Nausea and sickness are quite common side-effects of the general anaesthetic and painkillers. If you feel sick please let the nursing staff know as anti-sickness medicine is available to help reduce these symptoms and being unable to eat may slow down your recovery. You will be able to eat as soon as you feel like it. You will be given oxygen through a mask for a few hours.
Some discomfort or pain after surgery is normal. The nursing staff will assist you to control any pain through injections or tablets.
Your anaesthetist or pain nurse will discuss the best method of controlling your pain with you. There is a form of pain relief available called a PCA (Patient Controlled Analgesia). This means you will have a pump, which you control yourself to administer small doses of pain-killer by pressing a
button on the handset whenever you need more pain relief. It is very safe and you will be closely monitored by nursing staff. Another form of pain relief is an epidural. The anaesthetist inserts a thin hollow needle into the epidural space, just outside the outer covering of the spinal cord in the lower back. A small plastic tube is then introduced through the needle and left in position when the needle is removed. The tube is used to introduce local anaesthetic and pain killing medication. An epidural provides pain relief for as long as it remains in place, usually overnight. It may cause some temporary numbness and weakness in the legs, which wears off after three or four hours.
The Nursing Staff will assess you regularly to find out how comfortable you are. Suffering from pain can slow down recovery, so please tell the Nursing Staff if you are in pain at any time. While the pain may be acceptable when you are resting, it will increase when you move, and it is important to change position regularly and do exercises 5-6 times a day following the operation, so it is important to take pain relief regularly. We will be happy to help you in any way to make your stay as comfortable as possible.
You will probably be nursed on your back initially with your operated limb on a pillow for support. On the first day after your operation the physiotherapists will see you. They will show you some leg exercises to help with the circulation. If you feel well enough they will help you to sit onto the side of the bed and stand using a frame. You must follow the exercises given to you, contracting your thigh muscles, calf muscles and
moving your toes. If you feel soreness of your heel or tail bone (sacral area) you must tell the nurses. Various blood tests and x-rays will be taken and you may have a blood transfusion. On the second day after surgery the physiotherapists will help you get out of bed again and try a small walk with a frame. They will also encourage to start some knee bending exercises. Then on a daily basis you will practice your walking and as soon as you are able start using elbow crutches. If you have stairs at home the physio team will practice this with you to make sure you are safe to go home.
The occupational therapists will also see you to see if you require any equipment assistance for when you go home. You will be shown the safe way to:
• Sit
• Get on and off the bed
• Go to the toilet
Upon discharge from the hospital, you probably will have achieved some degree of independence in walking with crutches or a walker, climbing a few stairs, and getting into and out of bed and chairs. Nevertheless, you will need some help at home to assist you for a week or so. Get family to help with lower half garments or seek help from the Occupational Therapist or Physiotherapist for dressing gadgets. You may need to wear elastic (TED) stockings for six weeks after your operation.
The Community Intermediate Care Team is a team of Qualified Nurses, Health Care Support Workers, Social Services Staff, Rehabilitation Support Workers and Therapists who can support your discharge home following your knee replacement. It is our normal level of care to discharge you back to your own home as soon as it is reasonable to do so, usually 3 days after surgery and to provide you with the support you need at home. A member of the team will visit your home on the day after your discharge from hospital between 9am and 5pm to offer support and continue with treatment in your own home. They will provide the most appropriate care package for you, tailored to your individual needs. Not every patient will require therapy input. The team also works very closely with other colleagues in the community, such as District Nursing teams and Social Services and will liaise with these services if you require ongoing care and support in your own home.
It is important to continue with your exercises. The success of the operation has a lot to do with how well you do your exercises and strengthen your muscles. This part of your recovery is very much down to you. If excess muscle aching occurs, cut back on your exercises but do not stop.
Wound stitches or staples are removed on about the fourteenth day after surgery. The Community Intermediate Care Team will arrange for a District Nurse to visit you in your own home.
Upon returning home, you should be alert for certain warning signs. If you notice any swelling, increased pain, drainage from the incision site, redness around the incision, or fever, you should report this immediately to your doctor.
Whilst on bed rest, general exercises are very helpful.
These consist of:
1. Deep breathing and coughing to prevent post-operative chest infection following the anaesthetic.
2. Wiggling your toes.
3. Moving your feet up and down and tightening your calf muscles.
4. Tightening your thigh muscles.
5. Squeezing your buttocks together.
6. Bending and straightening your operated leg. To increase range of movement, you can help by using your hands.
7. Lying flat, brace your operated knee and lift the leg straight off the bed.
Get in and out of bed on the OPERATED side wherever it is possible. If your bed at home cannot be moved, take care not to let the leg roll in, as you get in and out. Sit down on the edge of the bed, push yourself further onto the bed and then keeping your legs TOGETHER and straight swing them onto the bed. Reverse the procedure when getting out of bed.
You will commence walking using a Zimmer frame or elbow crutches.
The sequence is always:
1. Walking aid moved first
2. then operated leg, and
3. finally, un-operated leg.
You can turn round either way (although your surgeon may advise you to turn away from your operated knee) but you must prevent pivoting or twisting your knee. Therefore, you must pick up your feet at each step making sure that the operated leg is not rotated too far in or out.
As your walking and confidence increase, you will usually progress to using two sticks.
The sequence will be:
1. Right stick, left leg
2. Left stick, right leg
It is advisable to sit in a high firm-backed chair with arms. You must feel for the chair with the back of your legs (a) and for the arms of the chair with your hands (b), sit down with your operated leg placed out in front of you taking the weight of your good leg (c and d).
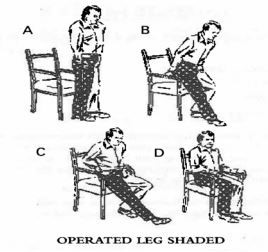
You will be taught how to do this by the Physiotherapist or Occupational Therapist. The same procedure is used for the toilet but with the aid of a raised toilet seat, if necessary.
Often your operated leg will be supported on a stool to prevent ankle swelling. Do not sit too long – if there is any ankle swelling it is better to rest on the bed rather than to sit. Always avoid low sofas etc… Do not turn or trust your body when standing on your operated let or sitting.
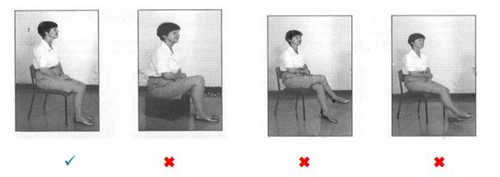
It is useful to use the opposite hand to the operated leg when putting on socks, stockings, etc. If you live alone the Occupational Therapist will assess you for dressing gadgets such a stocking aid or long-handled shoe horn.
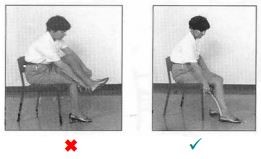
To retrieve fallen objects from the ground place your operated leg behind you and balance with your hand on a firm surface or stick bending forward from the waist and your good leg. If you live alone the Occupational Therapist will provide a “helping hand” to enable you to pick up items from the floor.
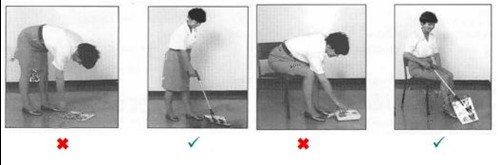
It is not advisable to get into a bath for 6 weeks. If you have a walk-in shower, this is ideal. If however there is a high step up to the shower you may need a block/small stool to help you get in and out. Bath seats and boards can be obtained from certain shops.
You will be taught how to negotiate stairs by the Physiotherapist. Banisters should be used with your free hand when possible:
Remember
1. Good leg leads up.
2. Operated leg leads down.
3. Stick stays with the operated leg.
Therefore, going upstairs:
1. Un-operated leg first.
2. Followed by operated leg.
And going down stairs:
1. Stick.
2. operated leg
3. and finally, un-operated leg
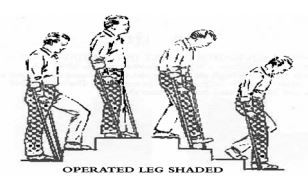
Getting in
1. Slide passenger seat back to give you as much leg room as possible.
2. Recline passenger seat to give you more room.
3. Put a cushion/pillow on the seat to raise it up a little higher.
4. Put a large plastic bag on the seat to help you ‘move’ easily (reduces friction) or wear a ‘shell’ suit.
5. Sit down bottom first using car door edge to steady you.
6. Grip both legs together or hook the foot of the un-operated leg under the operated leg or have someone to help you lift the leg into the car.
Turn 90° so both legs are on the ground outside the car. Use the car door edge to help you stand. Then have someone pass the crutches to you. Surgeons generally recommend that patients do not drive their car for a minimum of 6 weeks after the operation. You may be wise to alert your insurance company.
If you have ACUTE pain with swelling in the calf muscle, or swelling or wound redness at home, call your General Practitioner.
AVOID TWISTING THE OPERATED LEG WHEN WALKING, e.g. WHEN TURNING AROUND.
It depends on your job. It is possible to return at 8-10 weeks for those that do not perform manual work.
If at any time (even years after your surgery) you develop a bacterial infection such as sore throat or significant chest, urinary infection or cellulitis (redness and swelling of the limb) you should inform your General Practitioner of your hip replacement. Antibiotics should be administered promptly to prevent the occasional complication of distant infection localizing in the hip area. This also applies if you have any teeth extracted.
DO:
- Carry on with the exercises as instructed by your physiotherapist
- Take regular short walks
- Keep walking with your walking aids until 4 to 6 weeks after your operation. You will then progress to 1 walking stick held in the opposite hand to your new hip.
- Stand and sit as shown in hospital – operated leg in front, push on the arms of the chair, bed mattress or toilet seat frame
- Avoid pressure on the wound until it has fully healed and keep the wound dry until the skin has fully healed
- Avoid picking up objects from the floor or reaching down, unless you have been shown the correct method by the Therapist. Do not reach for objects when sitting, use a ‘helping hand’ for small objects. I f you live alone you will be given one.
- Go to your GP if you have an unusual pain, temperature, notice a discharge from your wound or any pain or swelling in your calves
- Please return any sticks or equipment when you have finished with them
- Ensure you take regular pain-killers for as long as you need to
- Eat a balanced diet with plenty of fresh fruit and vegetables
Until reviewed by your surgeon or a member of their team DO NOT:
- Twist the operated leg in or out whilst sitting or standing for at least 3 months
- Cross your legs, knees or ankles for at least 3 months
- Sit on low chairs, stools or toilets
- Drive a vehicle until advised it is safe to do so. Usually this is after 6 weeks if you can sit comfortably in your car and perform an emergency stop safely.
- Do any heavy lifting, housework or gardening
- Discard any walking aids until advised to do so
- Do too much too soon – gradually increase your activities as able.
- Return to work or sporting activities until advised to do so
Once you return home (in the first few weeks) if you have any questions or concerns that regarding your hip replacement call the Pre-operation Orthopaedic Clinic on (01782) 553216 if your operation was performed at the UHNM. Your General Practitioner can always advise on general matters and will tell you how to get further advice with the urgency the situation demands.
Ward 121 01782 553748
Ward 124 01782 552700
The Patient Advice and Liaison Service would be pleased to offer confidential advice and support if you have any concerns. PALS can be contacted on 01782 552814 or Email patientadvice.uhnm@nhs.net
Lumbar Discectomy / Decompression

This booklet is a guide to what you may expect when you are having discectomy or decompression surgery to relieve pressure on the nerve roots in your lumbar spine (lower back).
Your Surgeon will give you more detailed information, and will be happy to
answer any specific queries that you may have.
Intervertebral Disc -
The discs are the cushioning tissue which separate the bones of the spine
(vertebrae) and act as “shock absorbers”
Prolapsed Intervertebral Disc -
The disc herniates (pushes out) from its normal position, and as a result, can lead to pressure on the nerve leading to leg pain, pins and needles, numbess or weakness.
Sciatica -
This is the term given to pain down the leg. The pain is caused by irritation of the sciatic nerve - the main nerve in to the leg.

Stenosis –
This is the term given to the situation that results in pressure on the nerves due to a narrowing of the spinal canal. The commonest reason for this is due to wear and tear causing thickened ligaments, overgrown joints or bony spurs. This can lead to leg pain, pins and needles, numbness or weakness in your legs.

It is the surgical procedure to remove a prolapsed (bulging) part of the intervertebral disc in order to relieve the pressure on the nerve and hopefully alleviate leg pain. It is not an operation to relieve back pain, but can sometimes reduce some back pain.
It is the surgical procedure to remove pressure on the nerve roots in your spine due to thickened ligaments, overgrown joints or spurs of bone. It hopes to improve leg pain, and sometimes numbness and weakness. It is not an operation to relieve back pain, but sometimes can reduce it.
These operations usually are successful in 85-90% of patients that have
them. They are not always able to get rid of all of your symptoms, but do improve most of them. No operation is guaranteed, and all operations carry risks. Some of the risks with a spinal operation include:
General -
• Infection (less than 5% risk)
• Deep Venous Thrombosis (DVT) (less than 1% risk)
• Risk of serious life threatening or other complications due to allergies,
anaesthetics or bleeding are very rare (less than 1 in 1000)
Specific -
• Less than 1% risk of damage to the nerve involved leading to weakness
and/or numbness to the leg
• Less than 0.001% risk of major nerve damage which could lead to
problems with the bladder and bowels
• Around 1-2 % chance of leakage of spinal fluid through the wound. This
complication may need you to stay in hospital for longer, but can usually be corrected
• This operation is not performed to relieve back pain
It must be stressed that problems are rare and most patients are happy with the outcome of their surgery, but you need to be aware of the risks in order to give informed consent for the operation. Your surgeon will discuss all these risks with you in detail.
You may not have had all the tests listed or you may have had a test which is not listed. Your Consultant will decide which are appropriate for you. He will discuss if surgery is your best option and what alternatives are appropriate. Your name will then be entered on the Waiting List and you will receive a letter asking you to attend Pre-operative Assessment Clinic once you have been allocated an operation date.
At this appointment, you will meet the nurse responsible for taking a detailed history of your health and social support available to you.
What to bring with you -
• Any current medication or repeat prescription sheet
• A sample of your urine (you can obtain a bottle from your GP)
• Any scans or x-rays in your possession relating to your operation
What to expect -
• A time to discuss, in private, any worries or concerns you have with the nurse
• Further tests in preparation for your operation -
1. Blood tests
2. Urine test
3. ECG
4. Swabs from your nose and groin
All these tests are designed to give an overall picture of your health and
should problems be found, they can be dealt with quickly prior to surgery.
Some of the tests listed are done to minimise the risk of infection following surgery. Skin and urine infections, if found early enough, can be treated easily in a majority of cases with no need to postpone your operation.
• Meet the junior doctor who will perform a physical examination and confirm the medical history taken by the nurse. Your current medication will be discussed to identify any management needs before, during and after surgery. Any questions about the details and after-effects of your surgery can be discussed.
• A provisional date for surgery may be given to you and you will also be
sent a letter confirming your admission details.
• You may also see your consultant, who can answer any questions you may have. You might be asked to sign a ‘Consent to Surgery’ form at this
stage.
• A WRVS counter is available for the purchase of refreshments.
• The assessment process may take a few hours.
If you are unsure about going ahead with the surgery or your symptoms have improved, please bring this to the attention of the nurse. At no stage are you obliged to go with the operation, and your Consultant will be happy to discuss with you any concerns you may have.
You will receive a letter informing you of which ward you are to be admitted to and at what time if you were not given this information at your pre-operative assessment clinic appointment. You are often asked to come in on the day of your operation.
What to bring in -
• Your medication
• Scans and x-rays pertinent to your operation
• Nightwear
• Toiletries
• Towel
• Wet-wipes
• Juice drinks
• Light weight day clothes
• Sensible footwear
• Walking aids that you currently use
• Any sanitary products that you currently need
What to expect -
• You will wait in the Admission Lounge attached to the ward whilst your
pre-operative screening continues
• A nurse will re-check all the information documented from your previous
visits.
• All the results from the investigations carried out prior to admission will be checked and a further blood test will be Performed. The nurse will also check to ensure that all your scans and xrays are available.
• Your anaesthetist will discuss the anaesthetic that you are to receive.
• Once the Theatre List running order is available on the ward - the nurse can give you an approximate time that you can expect to go to theatre.
• All patients MUST fast prior to their operation. This is to minimise the risk of the stomach contents moving into the lungs when the anaesthetic is administered, a life-threatening situation. The nurse will advise you of the safe fasting time for you in relation to the time of your surgery.
• You will be measured for TED anti-embolism stockings on admission unless you have any skin condition that contra-indicates their use. These
are worn to minimise the risk of DVT and will need to be worn for approximately 6 weeks following your operation or until you are fully mobile again.
• Staff will discuss what you can expect whilst in hospital. Your relatives will receive information regarding visiting times and telephone numbers.
However, we recommend that you nominate 1 member of your family to
ring the ward and the rest of your family and friends ring that person. This
helps us to carry out nursing care instead of dealing with numerous
enquiries for the same patient.
• Before going to theatre, you will be asked to have a shower using antibacterial soap - to minimise the risk of infection.
• You may see your Consultant and be requested to sign a Consent to
Surgery form if you haven’t already done so.
Before your operation
What to expect -
• A visit from your anaesthetist (if not already seen)
• Fasting instructions MUST be followed or your operation may be cancelled
• You will have a shower in anti-bacterial soap then you will put on your
theatre gown and a pair of disposable pants. All your own clothes MUST
be taken off. All jewellery must be removed except for your wedding ring -
this can be taped in place to ensure that it will not be lost. Jewellery is
removed to prevent it from interfering with the equipment used in theatre.
• A porter will come and fetch you when it is your turn to go to theatre. You will be taken there on your bed and a nurse will escort you.
• You will proceed to the anaesthetic room where you will receive your
anaesthetic. Your anaesthetic will last for approximately 1½ to 2 hours and you will be lying on your front for your operation.
After your operation -
You may stay in Extended Recovery overnight following your operation, but this is not always necessary. Visiting is strictly between 7pm and 8pm and 2 visitors at any one time on Extended Recovery. Visiting is restricted in this area because theatre lists run until about 6.30pm and it is important for these patients to have privacy and confidentiality whilst they are recovering from their anaesthetic. Your visitors will need to report to ward 124 and staff there will be happy to show them to the Recovery area.
What to expect -
• You will be attached to equipment that monitors your pulse, heart rate and rhythm.
• The nurse will be monitoring your condition and asking you questions about how your current leg pain and movement compares to before the
operation.
• You may have PCA (patient controlled analgesia) in place. This is a system where you will give yourself a measured dose of morphine should
you feel any pain. There are safety measures in place to prevent you from
giving yourself too much morphine. The recovery nurses will explain how
to use the equipment and how to keep yourself as pain-free as possible.
We cannot guarantee that you will feel no pain but we will endeavour to
make you as comfortable as possible.
• If you experience any numbness, tingling or movement restriction to your legs, inform the nurse looking after you.
• You will be turned on your side regularly so that your wound can be
checked.
• Due to lying flat in bed, you may find that you are unable to pass urine. If this becomes a problem, you may require a catheter. This is a tube that is passed into the bladder to allow it to empty. The nurse will explain this in detail should a catheter be necessary.
• If you do not feel nauseous, you can have some water to drink. If this
doesn’t cause you to be sick, you may wish to try a light meal and a hot
drink.
• Some patients find lying flat uncomfortable. You may want to try sitting up a little or have a pillow placed under your knees. There is no problem with doing so unless your Consultant has specified that he wants you to stay lying flat initially. If you want to move into another position, the nurses will assist you to move in order to minimise pain.
• When sitting, it is important that you bend at the hips rather than bending your back, ensuring that a good, comfortable and safe posture is maintained.
You will be transferred to either ward 121 or ward 124 from Extended Recovery. The nurses on these wards will take over your care.
• If you have PCA, this will continue for the most part of this day
• You are advised to have regular tablet painkillers for at least 3 days. If the tablets have little effect, inform the nursing staff.
• Once on the ward, the physiotherapist will see you and assist you to get
out of bed safely. You will be helped to take a short walk on this day.
• If you needed to have a catheter after your operation, this will be removed at night-time.
• Regular checks are made of your wound dressing but it is not disturbed
unless absolutely necessary.
• You will have regular recordings of your temperature, pulse and blood
pressure.
• The Occupational Therapist will see you once you are able to walk safely.
• The physiotherapist will give you exercises to do at home.
You can plan to be in hospital until the day after your operation, but this can vary. Everyone is different, but 1- 2 days in hospital is a guide. Certain criteria have to be fulfilled before the doctor will allow you to go home.
You must -
• Be able to pass urine as you did prior to your operation
• Not have a high temperature
• Be able to eat and drink
• Be relatively pain-free
• Be able to walk unaided and negotiate stairs
• Be able to get on/off the toilet without difficulty
• Have no problems with your wound
This list should be used as a guide only. Your doctor or nurse will be able to answer any questions you may have. Always wait for the nurse to tell you that you are ready to go before you arrange for your family to pick you up.
You will need to have the following organised BEFORE you leave the ward -
• GP’s letter
• Outpatient appointment for approximately 6 weeks time
• Sicknote (if needed)
• Discharge medication
• Outpatient physiotherapy appointment if indicated
Once these are sorted out, you will be transferred to the Discharge Lounge to wait for your lift home.
Recovery - Expect to feel tired for at least 2 weeks after your operation but short walks are encouraged. You may still feel a degree of soreness in your back and you may still fell some pain in your leg. It is important that you take regular breaks in activity at this stage. By 4 weeks, you should be increasing your activity level as the pain and soreness decreases. By 6 -8 weeks after your operation, you should be feeling less tired and capable of leading a lifestyle which is your normal.
Wound - will be looked after by either your practice nurse or the District
Nurse. You can bathe once your wound has healed or if you have a waterproof dressing on the wound. However, we advise you not to sit down in the bath for a few weeks as you may find it too difficult to get in and out of it. Showers are easier to negotiate but you may wish for a member of your family to assist you initially in case you struggle.
Physiotherapy - if your Consultant wishes you to have outpatient physiotherapy, this will be arranged prior to your discharge.
Exercise - Short, frequent walks are encouraged. Your Physiotherapist will
discuss specific exercises with you which may benefit your recovery. You are advised not to go swimming for a few weeks, until your wound has fully healed.
Posture - Do not bend, twist or lift heavy objects. Continue to follow the advice of your Physiotherapist regarding sitting and keeping your back straight. You must use common sense and ask for advice regarding a certain activity if you are unsure if it is appropriate BEFORE you do it.
Driving - Generally, you may wish to avoid this for 4-6 weeks, but if you
feel comfortable sitting for a short time and are capable of doing an emergency stop, you may be fit to drive. Always check with your Insurance Company before driving for the first time following.
Sport – As a guide, most low impact sports can start again between 6-8
weeks after the operation. Swimming can usually start earlier, once the
wound has healed (2-4 weeks). Any high impact sports or sports that you
want to start fro the first time need to be avoided for 3 months. Ask your
consultant about any specific queries.
Work – As a guide, working from home can start between 2-4 weeks. Any
office work can start between 6-8 weeks. Work involving long distance driving or manual work may be best avoided for 8-12 weeks. Again your surgeon will guide you when you talk to them before the operation.