Common Sleep Problems
Obstructive Sleep Apnoea (OSA)
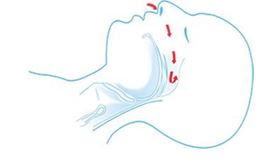
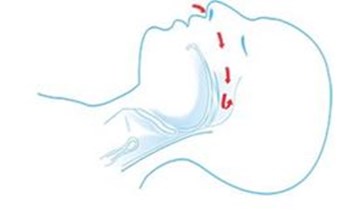
When you go to sleep your muscles relax, including those in your throat. In some people the relaxing muscles cause the airways to narrow. This can reduce the amount of air flowing in and out of your airways. This makes you snore.
If your throat closes completely, it causes you to stop breathing for a time. For it to be classed as an apnoea it needs to stop for at least 10 seconds. This results in your oxygen level in your blood falling.
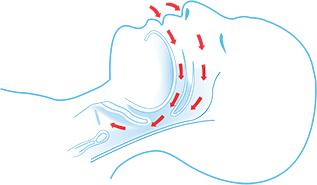
Normal airway
Collapsed airway in OSA
Your brain will detect this and wake you from your sleep. There is often a distinctive snort or grunt and some movement. This is only brief and you may not be aware of this happening, it results in poor quality, fragmented sleep. This often happens in cycles.
Dependent on the severity this could happen hundreds of times per night every night. There are certain things that can make OSA worse, for example, sleeping position.
Night-time symptoms
- Snoring
- Stopping breathing
- Waking up gasping / choking
- Acid Reflux
- Needing the toilet frequently during the night (Nocturia)
- Restlessness in bed
Often your bed partner is more aware of these symptoms.
Day-time symptoms
- Waking feeling un-refreshed
- Have a headache when you wake up
- Poor energy levels
- Poor concentration and less alert
- Falling asleep in appropriate places / times
- Low mood
- Low sex drive
OSA is more common if……
- You are middle aged male
- You post-menopausal female
- You are a woman in the later stages of pregnancy. OSA symptoms often improve or disappear after your baby is born
- You are overweight or obese
- Your collar size is larger than 17 inches
- You have a small airway, a set-back lower jaw or a small lower jaw, large tonsils, a large tongue or nasal blockage
OSA can be made worse by drinking alcohol, using sleeping pills and smoking or sleeping on your back.
Diagnosing OSA
By completing the STOPBang questionnaire (https://britishsnoring.co.uk/stop_bang_questionnaire.php) and the Epworth Sleepiness Scale (https://www.blf.org.uk/support-for-you/obstructive-sleep-apnoea-osa/diagnosis/epworth-sleepiness-scale) they may help you decide if you are at risk of OSA and how excessively tired you may feel during the daytime.
If you think you may have obstructive sleep apnoea it is important to consult with your GP. It can have a severe impact on your quality of life. OSA can be linked with various cardiovascular diseases such as, Stroke, high blood pressure, heart attack and diabetes. If you have a bed partner they may be able to report on what happens during your sleep.
Your GP / Specialist will refer you to the Sleep Clinic / Service.
The Sleep Clinic / Service are specialist clinics that assess, diagnose and treat people with a range of sleep problems, including OSA.
Once you’ve been referred, you will usually have an overnight sleep study at home to monitor your breathing, oxygen saturation and heart / pulse rate. This will help to diagnose OSA (link to test section).
If you are formally diagnosed with OSA, you may need to be started with CPAP treatment (link to CPAP section)
For more information on OSA visit the sleep apnoea trust information or useful links section.
Restless Leg Syndrome (RLS)
Restless legs syndrome, is a common condition of the nervous system that causes an overwhelming irresistible urge to move the legs. Over 80% of people with RLS also have a condition known as Periodic Limb Movement Disorder (PLMD) (see PLMD section)
Symptoms
It’s been described as:
- Tingling, burning, itching or throbbing
- A “creepy-crawly” feeling
- A feeling like fizzy water is inside the blood vessels in the legs
- A painful cramping sensation in the legs, particularly in the claves
They are unpleasant sensations and affect people with differing severity. It is usually worse in the evening and during the night, often relieved by rubbing or moving the legs.
Causes
Often an exact cause is not known for RLS, but the following are thought to contribute:
Dopamine – is a chemical on the brain, which helps control muscle activity and movement. Dopamine levels naturally fall towards the end of the day, this may explain why RLS symptoms are often worse in the evening and during the night.
Underlying health condition - where a pre-existing health condition may pre-dispose you to have RLS. This is known as secondary RLS and you could develop it with the following:
- Iron deficiency (leads to lower levels of Dopamine)
- Long term health condition such as Diabetes, chronic kidney disease, Parkinson’s and Rheumatoid Arthritis
- Pregnancy (particularly from 27 weeks to birth)
Triggers
There are several triggers, these do not cause RLS but can make it worse:
- Some medications such as:
- Antidepressants
- Antipsychotics
- Antihistamines
- Other possible triggers
- Being overweight
- Excessive smoking, caffeine and alcohol intake
- Stress
- Lack of exercise
Diagnosing RLS
There is no specific test for RLS, rather it is based on symptoms. Your GP should be able to diagnose it using these 4 criteria:
- An overwhelming urge to move your legs, usually with an uncomfortable sensation, as described earlier
- Symptoms occur or get worse when you are resting or inactive
- Symptoms are relieved by moving or rubbing your legs
- Symptoms are worse during the evening or at night
Treatment
Lifestyle changes can often lessen the symptoms of RLS, for example, reducing caffeine, alcohol and smoking, exercise more and good sleeping routine / habits (See sleep hygiene)
Avoiding the medications that may trigger RLS
Ensuring any underlying health conditions linked with RLS are treated adequately, for example, iron deficiency.
The following may also help during an episode of RLS to help relieve your symptoms:
- Massaging your legs
- Having a hot bath in the evening
- Applying hot or cold compress to your legs
- Doing activities that distract you from your leg muscles
- Relaxation techniques / exercises for example Yoga and stretching
Medication
Dopamine agnostics that may be recommended include:
- Ropinerols
- Pramipexole
- Rotigotine skin patch
Painkillers, such as codeine
A sleeping tablet, if RLS is disturbing your sleep
Further information can be found on the NHS website:
https://www.nhs.uk/conditions/restless-legs-syndrome/
Periodic Limb Movement Disorder (PLMD)
Periodic Limb Movement Disorder is repetitive cramping or jerking of the legs during sleep. It is the only movement disorder that occurs only during sleep, and it is sometimes called periodic leg (or limb) movements during sleep.
PLMD may occur with other sleep disorders. It is often linked with restless legs syndrome, but they are not the same thing (see RLS section)
PLMD can occur at any age and occurs in approximately 4% of adults. Like many sleep disorders, PLMD is more common in middle-aged and older people and female. It also occurs in shift workers and those who have irregular sleep patterns.
Symptoms
The most common symptom in a person with PLMD is not leg movement but reports of poor sleep and excessive daytime sleepiness. In most cases the patient is unaware of the leg movements and it is the bed partner that reports them.
Leg movements can involve one of both legs. Typically the knee, ankle and big toe joints all bend as part of the movements. The movements can either be very subtle to large and wild kicking and thrashing. The movements last approximately 2 seconds, they are rhythmic and repetitive, occurring every 20-40 seconds.
Causes
PLMD may be either primary (no known cause) or secondary (caused by an underlying health condition). It is possibly caused by abnormalities in the regulation of nerves travelling from brain the legs.
Secondary PLMD has various causes, and many are also the cause of RLS
- Diabetes mellitus
- Iron deficiency
- Spinal cord tumour
- Spinal cord injury
- Obstructive sleep apnoea
- Narcolepsy
- Uraemia - Build-up of waste products in the blood because of poor kidney function
- Anaemia
- Some medication
- Withdrawal from sedative medications such as barbiturates or benzodiazepines (such as Valium)
- Stress
- Excessive caffeine intake
Diagnosis
Blood test may be requested to rule out anaemia, deficiencies or metabolic disorders.
If another sleep disorder is suspected, you may be referred to the Sleep Clinic to undergo a sleep study, either at home or carried out in the sleep laboratory (see sleep study section) that will also incorporate sensors monitoring limb movements.
Treatment
As with RLS, treating the potential underlying cause such as anaemia may be sufficient. If PLMD is evident alongside OSA, treating OSA with CPAP often eradicates leg movements.
Clonazepam in particular, has been shown to reduce the total number of periodic limb movements per hour. It is probably the most widely used drug to treat PLMD.
Other medications that cause muscle relaxation may be used.
Further Information
https://www.nhs.uk/conditions/restless-legs-syndrome/symptoms/
https://www.rls-uk.org/periodic-leg-movement
REM Sleep Behaviour Disorder
REM sleep behaviour disorder (RBD) is a parasomnia. A parasomnia involves undesired events that happen while sleeping.
RBD occurs when you act out vivid dreams as you sleep. These dreams are often filled with action. They may even be violent. The episodes tend to get worse over time. Early episodes may involve mild activity. Later episodes can be more violent. This could result in injury of either the patient or their bed partner.
RBD episodes occur during rapid-eye-movement (REM) sleep. Normal sleep consists of a series of REM dream episodes, that occur about every 1 ½ to 2 hours each night. This means that an RBD episode tends to first appear at least 1 ½ hours after falling asleep. Episodes may continue to occur until waking up in the morning. Active RBD episodes may appear as many as four times per night. They may also occur as rarely as once per week or per month. RBD does not normally appear during a nap.
RBD can be confused with sleepwalking and sleep terrors. In these other disorders, the sleeper is usually confused upon waking up and would not be alert. In contrast, it is normally easy to wake a person with RBD who is acting out a dream. Once awake, he or she is also able to recall clear details of the vivid dream.
The details of this dream match the unusual behaviour of an RBD episode. These actions may include any of the following:
- Shouting
- Swearing
- Flailing
- Grabbing
- Punching
- Kicking
- Jumping
- Leaping
An RBD episode often disrupts the sleep of a bed partner. This is how a person with RBD may become aware of the problem. People with RBD are not more aggressive or violent than others when awake. RBD is a medical problem
Risk Factors
RBD most often occurs in men and can appear at any age, but it is most common in men after the age of 50 years. It occurs in less than 1% of the population
RBD is also seen more often in people with some neurologic disorders, occurring at a higher rate in those with:
- Parkinson’s disease (33%)
- Multiple system atrophy (90%)
RBD by itself does not cause the dreamer to be sleepy during the day. But it is often found along with other sleep disorders. These disorders may cause daytime sleepiness. Examples of these disorders include the following:
- Sleep apnoea
- Periodic limb movement disorder
- Narcolepsy
RBD can also be related to other factors that increase the intensity of REM sleep. These include the following:
- Alcohol withdrawal
- Sleep deprivation
- Brainstem brain tumours
- Stroke
- Use of certain medications
Episodes of RBD may increase due to the following:
- Sleep or REM sleep deprivation
- Other sleep disorders
- Alcohol
- Some medications
Treatments
RBD tends to respond to treatment with medications. Clonazepam is often used. However, treatment also requires the following:
- Bedroom safety precautions
- Maintain a normal total sleep time. Sleep deprivation will increase RDB
- Avoid certain medications and alcohol. They can cause or increase RBD
- Treat any and all other sleep disorders that will disrupt your sleep and increase RBD.
- Undergo regular monitoring for any neurologic symptoms. This includes tremor or other Parkinson symptoms.
Further information
For further information on RBD and other parasomnias, for example sleep walking, sleep talking or sleep paralysis
http://sleepeducation.org/sleep-disorders-by-category/parasomnias
Non-REM Sleep Behaviour Disorder
Non-rapid eye movement (NREM) Sleep Behaviour Disorder (NRBD) is a parasomnia. A parasomnia involves undesired events that happen while sleeping.
NRBD occurs during sleep, either during the entry into sleep, during sleep itself or during arousals from sleep. During a NRBD parasomnia there is a breakdown of boundaries between wakefulness and sleep. Meaning some areas of the brain are awake whilst some are simultaneously asleep during a NRBD event.
A normal sleep hypnogram – sleep structure – shows a transition from wake to transitional sleep (N1) to deeper transitional sleep (N2) to slow-wave sleep (N3) and finally REM sleep. This cycle takes approximately 90 minutes. N3 sleep occurs more frequently and for longer durations during the first half of sleep, whilst REM sleep occurs more frequently and for longer durations during the second half of sleep. NRBD occurs during N3 sleep and therefore, is more likely to occur in the first half of sleep.
NRBD is considerably more common in children, and frequently reduces or stops completely as the child enters adolescence and adulthood. However, a small percentage of the adult population experience NRBD.
There are four main types of NRBD are: confusional arousals; sleep walking; sleep terrors; and, sleep related eating disorders. Less common types of NRBD include: exploding head syndrome; sleep related hallucinations; sexsomnia, catathrenia (sleep groaning) and, sleep enuresis.
Symptoms
In many cases, NRBD does not result in symptoms. It is often identified by the disturbance it causes to bed partners and occupants of the household. However, NRBD may result in abnormally low N3 sleep which may result in daytime sleepiness.
Causes
NRBD is frequently caused by arousals from N3 sleep which can include: sleep disordered breathing (SDB); excessive noise; contact from bed partner; stress; and, periodic leg movement syndrome (PLMS). Less commonly, NRBD may be caused by: sleep deprivation, fever, sedatives, and alcohol.
Diagnosis
Diagnosis is almost exclusively achieved via a detailed medical history obtained from the patient and bed partner/other household occupants. A home/in-patient diagnostic sleep study may be useful, especially to rule out the presence of SDB and/or PLMS.
Treatment
Commonly, patients are provided reassurance on the benign nature of NRBD and that no treatment is required. Generally, efforts to curtail NRBD are often avoided. Environmental safety modifications especially in the presence of sleep walking, such as, removing dangerous objects, locking doors and windows and ensuring clear walkway are often recommended.
Improving sleep hygiene via ensuring a regular sleep cycle, sufficient amount of sleep, avoiding sleep deprivation, reducing stress and alcohol intake are encouraged. Alterations to medications, notably, sedative medications may occur.
NRBD may be caused by underlying sleep condition, such as, SDB and/or PLMS which will be treated accordingly.
Further Information
https://www.nhs.uk/conditions/sleepwalking/
Narcolepsy
Narcolepsy is a rare long-term brain condition, which causes a person to suddenly fall asleep at inappropriate times.
Narcolepsy does not cause long-term physical health problems, however, it can have a significant impact of daily life and mental health.
The brain had difficulty in regulating sleep and wake patterns which can result in the following:
- Excessive daytime sleepiness
- Suddenly falling asleep without warning
- Temporary loss of muscle control resulting in weakness and possible collapse, this is often in response to emotions such as laughter or anger. This is known as cataplexy.
- Temporary inability to speak or move when waking or falling asleep (sleep paralysis)
- Excessive dreaming and waking at night, dreams often comes as you fall asleep (hypnogogic hallucinations) or just before or during waking (hypnopompic hallucinations)
Causes of Narcolepsy
Narcolepsy is often caused by a lack of the brain chemical hypocretin (also known as orexin). This chemical is involved with the regulation sleep-wake cycle.
It is also thought that the lack of hypocretin is caused by the immune system mistakenly attacking the cells that produce it.
Genetic & Family history. Your risk of narcolepsy is 20 to 40 times higher if you have a family member who has narcolepsy.
Possible triggers of Narcolepsy include:
- Hormonal changes such as puberty or the menopause.
- Major psychological stress
- A infection, such a flu-like illness or a sore thorat
- The medicine used to vaccinated against it (Pandemrix)
Who can be affected by Narcolepsy?
Narcolepsy is a disability that affects around 1 in 2500 people or approximately 30,000 people in the UK. There is currently no cure, although medication and lifestyle changes can make life more manageable.
The symptoms of Narcolepsy often begin during adolescence, although it’s usually diagnosed between the ages 20 to 40.
Diagnosing Narcolepsy
If you think you may have narcolepsy, you will need to describe all your symptoms to your GP, maybe keep a diary, present this and your score on the Epworth Sleepiness Scale (https://www.narcolepsy.org.uk/resources/epworth-sleepiness-scale)
If you have cataplexy, you should emphasise this – with a video, if possible – as it is the most unusual of narcolepsy’s many symptoms. Your GP will need to refer you to a specialist sleep clinic or further tests. The is known as polysomnography (PSG)
It involves staying overnight at the Sleep Clinic so your sleeping patterns can be analysed.
During the night, several different parts of your body will be monitored using electrodes and bands that are placed on your body while you sleep (more information on PSG.
You may be asked to stay at the Sleep Clinic the following daytime to carry out another sleep test known as a Multiple Sleep Latency Test (MSLT). This involves keeping the electrodes and bands on from the night before (For more information on PSG and MSLT, click here)
Treatment
There's no specific cure for narcolepsy, but you can manage the symptoms and minimise their impact on your daily life.
Making some simple changes to your sleeping habits can sometimes help. If your symptoms are more severe, you'll usually need to take medicine.
Further information
Further information can be found, including treatments and living with Narcolepsy on the following websites:
https://www.nhs.uk/conditions/narcolepsy/
https://www.narcolepsy.org.uk/resources/what-narcolepsy
Circadian Rhythm Disorders
Circadian rhythm sleep disorders (CRSD) are a family of sleep disorders affecting the timing of sleep. Circadian rhythm is the name given to your body’s 24-hour “internal clock.” This internal clock controls your body’s sleep-wake cycle.
Helping to “set your internal clock” during a 24-hour day is the visual cue of light – specifically, its brightness / type of light, amount of time exposed to light, and when exposed to light.
If you suffer from a circadian rhythm sleep disorder, you may not be able to sleep and wake at the times required for normal work, school and social needs. If you are allowed to sleep and wake at the times dictated by your own body clock, you are generally able to get enough sleep.
Sleep is usually of normal quality unless there is another sleep disorder present.
There 6 CRSDs.
Delayed Sleep Phase Disorder (DSPD)
DSPD, often known as ‘night owls’ .This is characterised by an inability to fall asleep until 2-6 hours after usual sleep onset times (10pm to midnight) resulting in extreme difficulty with waking. When left to sleep, sleep length is generally normal or extended. DSPD has a prevalence of 7-16% in adolescents and young adults. Daytime functioning can be severely impaired by DSP. It can lead to excessive sleepiness and fatigue.
Advanced sleep-wake phase disorder (ASP)
People with ASP have an “early bird” circadian clock. They fall asleep several hours before a normal bedtime. As a result, they also wake up hours earlier than most people wake in the morning.
People with ASP feel sleepy in the late afternoon. Bedtime tends to occur between 6 p.m. and 9 p.m. Since bedtime is early, they also wake up early. They tend to wake up between 2 a.m. and 5 a.m. While the timing of sleep is early, sleep itself is normal.
Advanced sleep phase syndrome can affect both men and women equally but is more common in the elderly. Roughly 1% of people middle aged or older experience ASPS.
Non-24-Hour Sleep-Wake Syndrome
People who have non-24-hour sleep-wake syndrome (aka free running disorder) have a circadian rhythm that is out of sync. It causes these people to have slightly longer than 24-hour sleep cycles and causes their body clock to shift to later bedtimes every couple of days, making them go to sleep and rise at later times each day.
Non-24 hour sleep-wake syndrome is most common in blind people. As they are unable to regulate patterns of light and dark, therefore allowing the circadian rhythm to run free.
It is believed that as many as half of totally blind people suffer from the disorder. The disorder is less understood in sighted people suffering from non-24 hour sleep-wake syndrome.
Irregular Sleep-Wake Rhythm
This circadian rhythm sleep disorder occurs in people who have sleep-wake cycles that are not defined by any typical patterns of sleep. Instead, their sleep occurs as various "naps" throughout a 24-hour period that usually adds up to a normal sleep cycle of 7-9 hours. For these people there is no regular pattern and their nap times and durations can vary on a day-to-day basis.
Many sufferers of irregular sleep-wake rhythm complain of insomnia (because they can't sleep normally at night), excessive daytime sleepiness (because they feel the need to nap during the day), or both.
This circadian sleep rhythm disorder is extremely rare but is more prevalent in sufferers who have other medical or mental disorders such as dementia, brain damage, and mental retardation.
Shift-work sleep disorder
This occurs when a person's circadian rhythm conflicts with their work schedule causing them to experience insomnia or excessive daytime sleepiness. Shift-work is characterized by working hours outside of the traditional 9 a.m. to 5 a.m. schedule. It includes the early morning shift, late evening shift, the night shift, and rotating work schedules. Many people with set schedules such as early morning shifts and night shifts can adapt to their schedule if it is regular. However, people who work rotating schedules are at most risk as not having a regular schedule can wreak havoc on their circadian rhythm.
Jet Lag
Jet Lag occurs when a person quickly travels by plane to a new time zone, often one that is a few hours off from their home location. Jet leg most often occurs 2 time zones away from home. At the new location the person has to adjust to a new sleep-wake cycle that is at odds with their circadian rhythm. Jet lag is often harder to adjust to during eastward travel, as the new schedule requires earlier awakenings rather than later ones.
Jet lag is often a temporary disorder and the new time zone can be adapted to within a few days. However, jet lag disorder can be more serious for frequent fliers whose jobs require constant travel. Jet lag is often more difficult for the elderly to adapt to than the young.
Diagnosis
Keeping a diary of your sleep, including bed wake times is a useful way of tracking sleep patterns. Your GP may refer to the Sleep service.
An overnight sleep study is not usually required, however movement can be monitor using a special type of wrist watch, called an ActiWatch. This is usually worn for a 3 week period alongside a sleep diary. This will show the specialist if there are patterns of movement and when they occur.
Treatments
Behaviour Therapy
Depending on the circadian rhythm disorder, certain behavioural or lifestyle remedies may help alleviate symptoms of the disorder.
- Maintaining regular sleep-wake times
- Avoiding naps
- Getting regular exercise
- Avoiding caffeine and nicotine before bed
- Adjusting exposure to daylight. Those with delayed sleep phase syndrome should minimize exposure to electronics that mimic daylight (laptops, TV’s, cell phones, portable game consoles, etc.) and those with advanced sleep phase syndrome should increase light exposure in the evenings.
Bright Light Therapy
Light therapy can be used to help advance or delay sleep through the use of a high intensity lightbox. Bright light therapy helps in calibrating the circadian rhythm by having the user sit in front of the bright light box at appropriate times of the day (depending on the disorder being treated) for a varied amount of time (depending on doctor recommendations).
Medications
Certain medications may be prescribed depending on the type of disorder. Wake promoting agents or sleeping aids may be prescribed.
Melatonin, the hormone that helps regulate sleep, may be prescribed to be taken at certain times to help reset your internal body clock.