Living well
- Prehabilitation (prehab) means getting ready for cancer treatment in whatever time you have before it starts. It is a programme of support and advice that covers five particular parts of your health:
- What you're eating and your weight
- Breathlessness
- Physical activity or exercise
- Smoking
- Mental wellbeing
Cutting down on alcohol can also help, while you're having treatment, with your recovery, as well as improving your overall health.
It is very common for people with lung conditions to experience loss of appetite and weight. This might be due to the condition itself, the medications you are offered or the feelings associated with your experience.
It is really important to try and maintain a balanced diet with plenty of calories during this time.


Eating Well Roy Castle information - www.roycastle.org/about-lung-cancer/living-with-lung-cancer/eating-well/
Macmillan build up diet digital - www.be.macmillan.org.uk/be/p-26168-the-building-up-diet.aspx
Breathlessness is an unpleasant sensation of uncomfortable, rapid or difficult breathing. People say they feel puffed, short of breath or winded. The medical term is dyspnoea. Your chest may feel tight and breathing may hurt. Everyone can experience breathlessness if they run for a bus or exert themself to an unusual extent.
Improving breathlessness can improve your future cancer treatment options.
https://www.youtube.com/watch?v=1XxzHT7mxvQ Cambridge breathlessness video
- Conditions of use
- The BTF model image and animation are free to use with the following conditions:
- 1. The image and animation cannot be amended or adapted in any way.
- 2. The following statement needs to be included with the image or animation:
- Reproduced with permission of the Cambridge Breathlessness Intervention Service.
- 3. The following reference needs to be cited:
- Spathis A, Booth S, Moffat C, Hurst R, Ryan R, Chin C, et al. The Breathing, Thinking, Functioning clinical model: a proposal to facilitate evidence-based breathlessness management in chronic respiratory disease. npj Primary Care Respiratory Medicine. 2017;27(1):27.
Prehabilitation on the lung cancer pathway - Breathing techniques to help with breathlessness
Introduction
The information provided in this leaflet is designed to help you manage your longstanding breathlessness.
Please seek advice from your GP if you feel your breathing is getting worse or you experience being breathless as a new feeling.
Muscles involved in breathing
The diaphragm
The main muscle for breathing is called the diaphragm. This flat sheet covers the bottom of your rib cage.
- As you breathe in, the diaphragm moves down to help pull air into your lungs and your tummy rises and pushes out.
- When you breathe out, your diaphragm relaxes, returning to its natural dome shape, allowing your stomach (tummy) to rest in.
- Breathe gently when practising. There should only be a slight movement of your abdomen at rest.
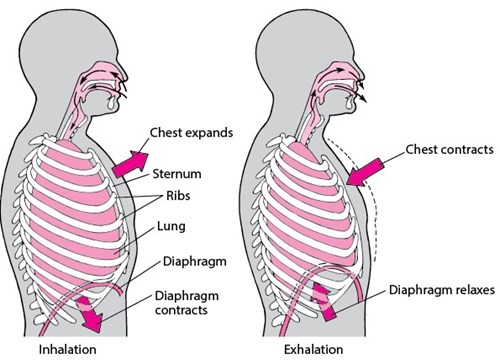
Breathing accessory muscles
Muscles in your neck, chest and shoulders move your neck and arms. When you are breathless, these muscles pull on your ribs to help with breathing. These are called ‘accessory muscles’.
Breathing techniques
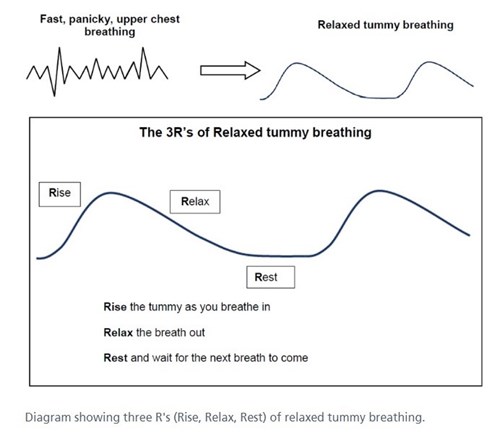
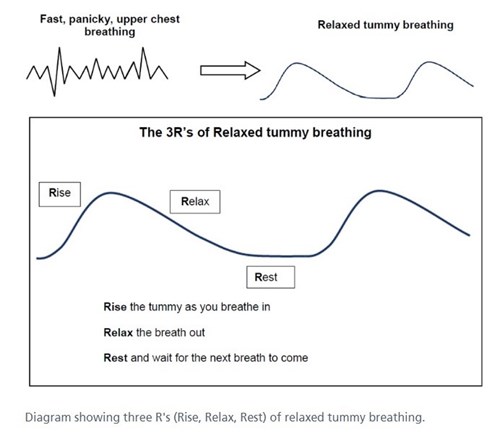
‘Relaxed Abdominal (Tummy) Breathing’
- You can use this technique with a fan and a position to ease breathlessness.
- Relaxed abdominal/’tummy’ breathing can help you recover quicker from breathlessness after activity and also help your breathing to settle if you feel anxious.
- Relaxed breathing is sometimes known as ‘breathing control’. The aim is to move from fast, upper chest breathing to relaxed, slow ‘tummy’ breathing.
- This technique helps to make your breathing more effective by focusing on breathing from your diaphragm with the upper body relaxed.
- Breathing from the abdomen does not always come naturally. You can practice relaxed breathing when you are not breathless for 10 minutes at a time, at least twice a day.
- Before practising, make sure you are in a comfortable position with your head and back supported and your shoulders and upper chest relaxed.
- Place one hand on your abdomen.
- Feel the abdomen rise and expand as you breathe in and relax down as you breathe out.
- If you have a tendency to breathe with small fast breaths from the top of your chest, you may find taking slower, deeper breaths from your abdomen helps to ease breathlessness.
‘Breathe low and slow, relax, let go’
‘Wave breathing’
When practising abdominal breathing, some people like to imagine a wave.
‘Breathe a rectangle’
Some people may prefer the idea of ‘breathing a rectangle’.
- Wherever you are, you can often see a rectangle, for example a book, TV, computer or tablet screen, a door, window, table top, or picture on the wall.
- Follow the sides of the rectangle with your eyes as you ‘tummy’ breathe. Slow down the speed at which your eyes move around the edge of the rectangle to slow your breathing.
- Breathe in on the short sides and breathe out on the longer sides
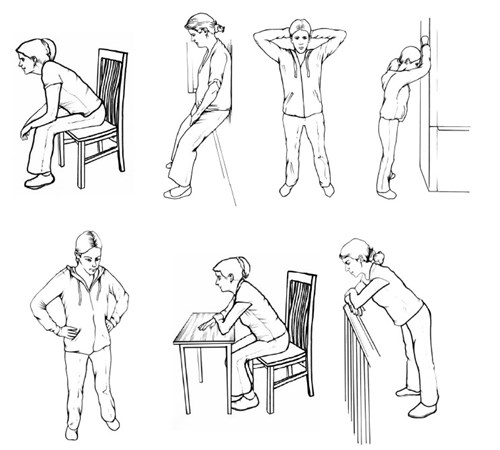
‘Recovery breathing’
- Use recovery breathing when you feel extremely breathless or anxious and you cannot use relaxed abdominal/’tummy’ breathing.
- Recovery breathing allows more time for the air to leave your lungs as you breathe out, making more room for the next breath in.
- The aim of recovery breathing is to calm your breathing until you can breathe smoothly and quietly from your tummy again.
The ‘three Fs’ of Recovery breathing
- Fan
- Forward leaning position
- Focus on long or relaxed breaths out
People with COPD and asthma may prefer long breaths out, sometimes through pursed lips.
Pursed lips breathing
Some people find breathing in through the nose and out through narrowed lips helps to ease their breathlessness.
- This technique can help people who have conditions such as COPD/ Emphysema.
- People who find this technique helpful will sometimes use it without realising they are doing it.
- ‘Pursed lips breathing’ helps to keep the airways to open, allowing air to leave the lungs more easily. This creates more room for the next breath in.
- You can use ‘pursed lips breathing’ at the same time as relaxed tummy breathing or recovery breathing.
General advice
Avoid holding your breath during activities when you tend to experience breathlessness, such as climbing stairs or bending down.
- Try to ‘blow as you go’, which means breathing out on effort. Blow out when bending, lifting, reaching or standing up from a chair
- Please do not rush.
- Pace your breathing with your steps. Take a breath in and out on each step when climbing the stairs.
- Some positions may help to ease breathlessness after you have been active.
- With all positions, try to relax the hands, wrists, shoulders, neck and jaw as much as possible.
- Experiment with your arm position to find which position suits you.
Your general health and well-being can be improved by small increases in your daily levels of activity. These small changes can improve your future treatment options.
This might be achieved by walking for a few more minutes every day or by doing chair-based exercises.
Why quit?
Stopping smoking is good for everyone. It’s even more important if you have a pre-existing health condition or a potential lung cancer. Treatment is safer and works better for those who have been able to stop smoking; symptoms and quality of life are also improved by stopping smoking. (Global Lung Cancer Coalition, 2017).
Smoking decreases the level of dopamine (happy hormone) in your brain, if you stop smoking this level will return to normal and there are medications available to help you during the transition period. As well as Nicotine, cigarettes contain many toxic chemicals, these increase the risk of many diseases long-term and smoking during treatment for lung cancer significantly increases the risk of complications, doubling your risk of dying after surgery! This is why it is so important to stop now and we are here to help you.
Help giving up smoking | Help giving up smoking | Stoke-on-Trent
Stop Smoking - Everyone Health Staffordshire
Quit smoking - Better Health - NHS (www.nhs.uk)
Stop smoking – Roy Castle Lung Cancer Foundation
Smoking | Asthma + Lung UK (blf.org.uk)
Vaping and e-cigarettes | Asthma + Lung UK (blf.org.uk)
Low mood and anxiety is common for people to experience anxiety and other symptoms and conditions relating to mental health. These can be heightened during this process.
Cancer and your emotions | Macmillan Cancer Support
Managing your mental health and lung cancer – Roy Castle Lung Cancer Foundation
What is cancer fatigue? | Coping physically | Cancer Research UK
Staffordshire and Stoke-on-Trent Wellbeing Service (staffsandstokewellbeing.nhs.uk)