Investigations
CT SCAN
IMPORTANT GENERAL POINTS:
- In many cases you will be asked to drink either water or a specialised liquid to outline the bowel before your scan: this will not delay your scan time, you will have been asked to come early for this purpose.
- A full bladder is not essential for every scan so if you need to go to the toilet please ask a member of staff.
- You may be in the CT department for up to 2 hours so please ensure you allow for this when planning your day and paying for car parking.
- We do our best to keep to time and always try and keep patients informed if there are any delays. However, if you feel that you have waited a long time and would like to check on your scan time please speak to member of the radiology staff.
- Please Inform a member of staff you have had a previous allergic reaction to x -ray dye or could be pregnant.
- Remember the scan itself is only half the story. If you have not heard from the hospital or your GP after 4 weeks please make contact with them and ask for your scan results.
BEFORE YOU COME:
Imaging Helpdesk number 01782 679285
- Please contact us on the number above If you think you might be pregnant.
- Please tell us before you come if you have any special needs such as
- Wheelchair access
- Interpreter
- Difficulties with eyesight or hearing Significant mobility problems
- If you think you will need assistance changing into a gown please bring someone with you who can help.
WHAT IS A CT SCAN?
- CT means computerised During the test you will lie on a special table that will move slowly through the scanner. As you move, the scanner will rotate around you taking pictures using x-rays. This information is then processed by a computer and used to build images which show your body in cross section or "slices".
- A CT scanner can see areas of your body that are not seen on ordinary x-rays. The scanner is shaped a bit like a doughnut or polo.
CAN I BRING A RELATIVE OR FRIEND WITH ME?
- You are very welcome to bring someone with you, especially if you think you will need help with getting changed into a gown or if you think you will need help understanding additional information you may be
- Your friend or relative will not be allowed into the scan room with you unless there are exceptional circumstances.
- Please note children will not be allowed into the scan room so please make arrangements for them before you come to your appointment.
WHAT DO I DO ON THE DAY OF THE SCAN?
- Book in at reception and take a seat in the waiting
- Some scans do not require special preparation but PLEASE NOTE IN SOME CASES YOU MAY BE ASKED TO SIT AND DRINK SOME WATER OR A SPECIAL CONTRAST DRINK FOR AT LEAST 30 MINUTES BEFORE YOU GO IN especially if you are having an abdomen or pelvis scan.
- Please refer to you appointment letter for specific preparation instructions.
- You may be asked to change in to a gown. We advise that where possible you leave valuables at home.
WHO PERFORMS THE SCAN?
- Your scan will be performed by a specially trained radiographer who works closely with a Radiologist (a doctor who specialises in looking at CT scans and x-rays) to produce the best scan possible for your individual
- When your scan is finished the radiologist will study the images carefully and will then make a written report which is sent to the doctor who requested your test.
- The radiographer will be close throughout your scan, explaining everything to you and answering any questions that you may have.
WILL I NEED AN INJECTION?
- It may be necessary to put a small plastic tube (cannula) into a vein in your arm: this is because sometimes we need to give an injection of a special x-ray dye (contrast medium) to outline the blood vessels more clearly to increase the amount of information we can get from the If this is necessary everything will be explained to you at the time and you will have the opportunity to ask questions before the scan goes ahead.
- The Injection may give you a warm feeling around your body and a metallic taste in your As with all injections there is a small risk of an allergic reaction ranging from a minor reaction such as a skin rash to a more serious reaction such as an asthma attack. Our medical teams are trained to deal with any sort of allergic reaction if it should happen.
If you have had an allergic reaction to an x-ray dye before such as for coronary angiography or a previous CT scan please let the radiographer know.
WHAT HAPPENS DURING THE SCAN ITSELF?
- In the scan room you will be asked to lie on the scan During the scan the table moves slowly through the scanner taking x-rays as it goes along. You will need to keep very still and may be asked to hold your breath while the pictures are taken.
- The scan itself takes between 5 and 10 minutes but you may be in the department for up to 1 and 1/2 hours so please allow time for this.
ARE THERE ANY SIDE EFFECTS?
- There are no known side effects from having a CT scan, however there is a very small risk of a delayed allergy-like reaction to the x-ray dye (contrast medium).
- If you do develop any symptoms and are concerned, please contact us for advice, or contact your GP.
- A CT scan involves a small dose of radiation but all steps are taken to keep the dose as small as Radiation can cause health problems in high doses: rest assured that the doctor who has asked for you to have the scan and the radiology team in the CT department feel it is important for the scan to go ahead to make a diagnosis or sometimes to monitor the effects treatment you are having.
WHAT HAPPENS AFTER THE SCAN?
- Once the scan is finished the CT staff will check that they have all the Information they If you have had a cannula put in, someone will come and remove It. You will then be able to leave the department. You can go back to normal activities straight away.
- If you are diabetic and taking metformin it may be necessary for you to stop taking it for 48 hours after your The radiographer doing your scan will Inform you if you need to do this.
HOW DO I GET MY RESULTS?
Remember, your scan is only half the story, your results are the other half. A full written report will be sent to your doctor whom you will be required to see to get your results. If you have not heard anything after 3 weeks, please contact the doctor who referred you for your scan.
CONTACT US
If you:
|
- have any queries or concerns about your appointment or the preparation for your procedure
|
suffer with dyslexia or have visual problems and require this patient Information leaflet with a different background or font we can send this to you on request
need an Interpreter or have other special circumstances that we can help you with such as hearing or sight problems or difficulties with mobility
Contact the imaging helpdesk on 01782 679285
If you need to cancel or re-arrange your appointment please e-mail us on
imaging.appointments@uhns.nhs.uk
Your feedback is important to us: we would like to hear any feedback (good or bad) via one of the following routes:
- E-mail us on feedback@uhns.nhs.uk
- Fill out a comment card (available in all waiting areas or ask a member of staff) and put it Into one of the comment card boxes at the entrance to the department you are in.
Complete a patient satisfaction survey: this will be handed to you If you come during a survey period or can be requested from the reception staff or via the UHNM website: go to uhnm.nhs.uk/OurServicces/pages/Imaging.aspx
- If you would be willing to be contacted to be Involved In a patient advice and liaison please send your email address to imagingpatient.feedback@uhns.nhs.uk
Data sharing: Any personal information is kept confidential. There may be occasions where your information needs to be shared with other healthcare professionals to ensure you receive the best care possible. In order to help us improve the services we provide your information may be used for clinical audit, research and teaching but will always have all personal information removed.
MRI
PET CT scan patient information leaflet
PFT
ECHO
WHAT IS A CT GUIDED LUNG BIOPSY?
A CT guided lung biopsy is a procedure used to take a small piece of lung tissue from an abnormal area seen on a previous CT scan. The sample is then examined under a microscope.
The biopsy will be performed using CT scan guidance to position the needle accurately into the abnormality.
WHAT ARE THE BENEFITS OF HAVING A LUNG BIOPSY?
Having a biopsy will help your doctor to make a correct diagnosis so that you can get suitable treatment.
WHAT ARE THE RISKS OF HAVING A LUNG BIOPSY?
- There may be bruising or a small swelling around the biopsy area due to bleeding into the skin. This should not be painful and will heal.
- Air may leak out of your lung: this is called a pneumothorax. If this happens, you may feel short of breath or experience some chest pain. You may not need treatment for this, but rarely a small drain (tube) has to be inserted through the skin to relieve the air leak and this may mean you need to stay in hospital
- There is also a small risk of coughing up a small amount of blood during or after the procedure. This is rarely a large enough amount to be considered dangerous and you will be closely monitored at all times.
- Unfortunately, some biopsies fail to give an answer. This may be because despite taking every possible care, the tissue sample is from an area of normal rather than abnormal tissue, or it is not enough for the histopathologist to make a definite diagnosis.
ARE THERE ANY ALTERNATIVES?
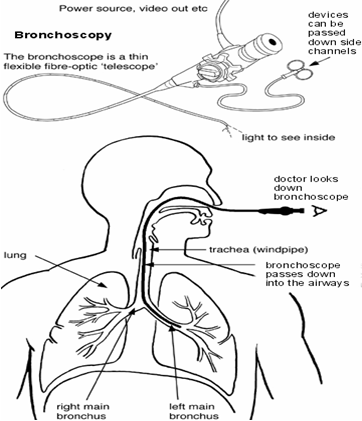
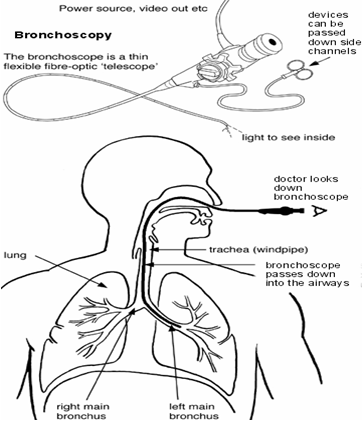
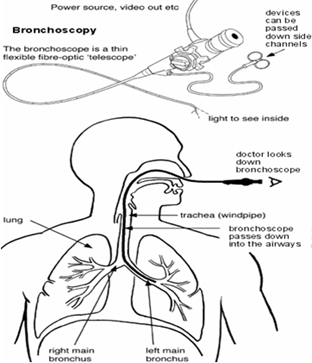
Sometimes a tissue sample can be obtained using a thin telescope with a biopsy needle on the end (bronchoscopy). This is only appropriate in some cases and depends on where the abnormality is in relation to the main airways. Your doctor and the radiology team have looked at your scans in detail and feel that this procedure is not suitable for you.
A lung biopsy is the only way for your doctor to get the information needed to make a correct diagnosis.
WHO WILL BE PERFORMING THE BIOPSY?
A consultant radiologist will perform the CT guided biopsy. A radiologist is a doctor who has undergone further training in the use of imaging and interventional biopsy techniques.
You will meet the radiologist who will be carrying out the biopsy. He/she will tell you about the procedure and will answer any questions you may have. You will then be asked to sign a consent form.
If you have any allergies or have had a previous reaction to contrast medium (dye to enhance CT scan pictures) you must tell the radiologist before the procedure starts.
You will be asked to lie on the scanning table and the radiologist will decide which position is the best for you to lie in for the biopsy. Pictures taken will be used to direct the radiologist to the exact place suitable for inserting the biopsy needle.
The skin will then be cleaned with an antiseptic solution and local anaesthetic will be injected into the skin before the biopsy needle is inserted. The local anaesthetic can sting a little but this soon wears off and the area will feel quite numb.
A needle will then be inserted into the abnormal area and a small tissue sample obtained and sent to the pathology department to be analysed. It will take the pathologist several days to examine the biopsy specimen therefore do not expect to get the results until the following week.
WHAT HAPPENS AFTER THE BIOPSY?
You will be taken to a ward where you will be asked to stay in bed for a few hours, until you have recovered from the procedure. Nurses will carry out routine observations such as taking your pulse and blood pressure to make sure you are all right.
A chest x-ray will be taken approximately 2 hours after the biopsy and if all is well you can then go home.
Please arrange for someone to drive you home or accompany you in a taxi as driving is not advised for 24 hours. We do not recommend that you use public transport as it is unsafe if you feel unwell.
WHEN WILL I GET THE RESULTS?
The results will take about seven to ten working days. You will need to make an appointment to see the doctor that referred you in order to discuss the findings of the biopsy and any further treatment that you might need. If you have not been contacted with a follow up appointment within 2 weeks please contact the secretary of the Consultant who referred you for the procedure.
WHAT DO I NEED TO DO AFTER I GO HOME?
You should rest for the remainder of the day and possibly for the next day, depending on your recovery.
Have someone to stay with you overnight
- Eat and drink normally
- Take your usual pain relief, as prescribed, if you have any pain
- Continue with your normal mediation as prescribed
- Keep a regular check on the biopsy site
Information may be used for clinical audit, research and teaching but will always have all personal information removed.
Endobronchial Ultrasound-guided Transbronchial Needle Aspiration (EBUS-TBNA)
What is EBUS-TBNA?
EBUS-TBNA is a safe and effective technique that allows the doctor to look into your lungs and take samples of the lymph glands located in the chest. Lymph glands (sometimes called lymph nodes) are an important part of the immune system and are joined together by lymph channels; they are normally pea-sized.
A thin flexible tube (bronchoscope), which is smaller than the diameter size of a little finger, is passed into your mouth to look directly into your lungs. The bronchoscope is combined with high frequency sound waves, transmitted from the ultrasound probe at the tip of the bronchoscope. This allows a scan of the surrounding lymph glands; these glands are located outside the breathing tubes and a fine needle is used to take samples.
It is a day case procedure, done under sedation and local anaesthesia.
 Patient.co.uk
Patient.co.uk
What are the benefits?
The lymph glands in the chest may become enlarged for a variety of reasons. Taking samples from the lymph glands will help us determine the underlying diagnosis in 9 out of 10 cases. Occasionally, another test may be required.
What are the risks?
- EBUS is generally a very safe procedure with risk of serious complication being 1 in 1000.
- Minor complications include cough, sore throat, hoarse voice and lung collapse.
- Occasionally you may cough up small streaks of blood; this usually settles in a day or two. Should it be a large amount or if you feel unwell, please report to the nearest Hospital Accident and Emergency Department.
Preparation prior to the procedure
- You must NOT have anything to eat for at least 6 hours prior to procedure but you may drink clear fluids such as water, black tea or coffee up until 2 hours before the test.
- If you are on regular medications please take your tablets as normal with a sip of water.
- If you have allergies to any medications, please inform us.
- For Patients taking blood thinning medications (anticoagulants and antiplatelets):
Please inform us if you take Warfarin, Clopidogrel, Direct oral anti-coagulants (Rivaroxaban, Apixaban, edoxaban, dabigatran) Prasugrel, Dipyridamole or other blood thinning treatments including injections (eg. Low molecular weight heparins: Dalteparin) as these may need to be temporarily stopped before the bronchoscopy with a view to reduce the risk of bleeding during or after the procedure.
Risk and benefit of withholding or stopping the above treatment will be discussed prior to procedure.
For Patients who take insulin for diabetes:
Your medication may need to be altered therefore, please contact your diabetic nurse 3 days before the procedure for advice.
Diabetic Nurse 01782 679770 Monday - Thursday 0900 to 1630; Friday 0930 to 1600.
If you take oral tablets to control your diabetes such as Metformin, please do not take them on the morning of the procedure.
On the day of the procedure
- Please bring a copy of your prescribed medication with you on the day of your procedure.
- Please inform the receptionist at the Endoscopy Unit on arrival.
- You will be seen by a member of nursing staff who will check your details and assess your blood pressure and oxygen levels.
- You will then be seen by a doctor who can answer any questions you may have and request you to sign a consent form for the procedure.
Sedation
- It is usually necessary to have sedation but you will not be “put to sleep”.
- You will be given an injection into a vein in the back of your hand or your arm.
- This will help you relax and make you more comfortable; you may not remember anything about the procedure afterwards.
- If you have been given sedation, you must not drive, operate machinery, drink alcohol or sign any legally binding documents for 24 hours after the procedure.
What happens during the procedure?
- Local anaesthetic spray will be applied to the back of the throat and/or local anaesthetic jelly to the nostrils; these may taste unpleasant.
- The doctor will then gently pass the bronchoscope to look inside the airways and take samples as required; you may be offered more anesthetic or sedation to help address any discomfort you may feel during the procedure.
- If necessary, the doctor may take a ‘photograph’ of any abnormalities seen within the airways.
How will I feel during the procedure?
- The procedure will not hurt you and you will be able to breathe normally during the procedure.
- It may make you cough as the bronchoscope goes into your airways.
Immediately after the procedure
- Post procedure you will be monitored for at least two hours prior to discharge.
- As your throat will have been numbed, your swallowing will not be normal and therefore it is NOT safe to eat and drink for up to two hours.
When do I know the results of the procedure?
- If samples have been taken, the results may take up to a week.
- The details of the results and necessary treatment will be discussed with you by the referring doctor.
What support will I need post procedure?
If you live on your own, you will need to arrange for someone to stay with you overnight after the procedure, however if you are unable to arrange someone to stay with you overnight after the procedure, we may have to admit you for overnight stay in the hospital. You will also need someone to drive you home.
Further Information:
If you have any further queries after the procedure please contact
Bronchoscopy coordinator
Respiratory Department
Royal Stoke University Hospital
University Hospital of North Midlands NHS Trust
Telephone number: 01782 675760
Monday to Friday 08.30 hours to 16.30 hours
Outside of these hours please contact your GP surgery for the telephone number for the emergency doctor’s service.
What is a Bronchoscopy?
- A bronchoscopy or a camera test is a procedure by which a doctor can examine the airways in your lungs.
- The bronchoscope is a thin flexible tube with a bright light and camera at the end which is passed through your nose (or mouth) and down into the airways.
- It allows examination of the airways and to obtain tissue samples for further testing.
What are the benefits?
Bronchoscopy is performed to diagnose and to treat various lung conditions.
- To look into the cause of abnormal areas within the airways or an abnormal patch on the lung.
- To investigate symptoms such as cough (including coughing blood) and breathlessness.
- To clear secretions (or remove foreign body) from the airways and take samples to look into the cause of lung infection.
What are the risks?
- Bronchoscopy is generally a very safe procedure with the risk of serious complication being 1 in 1000.
- Minor complications include cough, sore throat, hoarse voice and lung collapse.
- Occasionally you may cough up small streaks of blood; this usually settles in a day or two. Should it be a large amount or if you feel unwell, please report to the nearest Hospital Accident and Emergency Department.
Preparation prior to the procedure
- You must NOT have anything to eat for at least 6 hours prior to procedure but you may drink clear fluids such as water, black tea or coffee up until 2 hours before the test.
- If you are on regular medications please take your tablets as normal with a sip of water.
- If you have allergies to any medications, please inform us.
- For Patients taking blood thinning medications (anticoagulants and antiplatelets): Please inform us if you take Warfarin, Clopidogrel, Direct oral anti-coagulants (Rivaroxaban, Apixaban, edoxaban, dabigatran) Prasugrel, Dipyridamole or other blood thinning treatments including injections (eg. Low molecular weight heparins: Dalteparin) as these may need to be temporarily stopped before the bronchoscopy with a view to reduce the risk of bleeding during or after the procedure.
Risk and benefit of withholding or stopping the above treatment will be discussed prior to procedure.
For Patients who take insulin for diabetes:
Your medication may need to be altered therefore, please contact your diabetic nurse 3 days before the procedure for advice.
Diabetic Nurse 01782 679770 Monday - Thursday 0900 to 1630; Friday 0930 to 1600.
If you take oral tablets to control your diabetes such as Metformin, please do not take them on the morning of the procedure.
On the day of the procedure
- Please bring a copy of your prescribed medication with you on the day of your procedure.
- Please inform the receptionist at the Endoscopy Unit on arrival.
- You will be seen by a member of nursing staff who will check your details and assess your blood pressure and oxygen levels.
- You will then be seen by a doctor who can answer any questions you may have and request you to sign a consent form for the procedure.
Sedation
- It is usually necessary to have sedation but you will not be “put to sleep”.
- You will be given an injection into a vein in the back of your hand or your arm.
- This will help you relax and make you more comfortable; you may not remember anything about the procedure afterwards.
- If you have been given sedation, you must not drive, operate machinery, drink alcohol or sign any legally binding documents for 24 hours after the procedure.
What happens during the procedure?
- Local anaesthetic spray will be applied to the back of the throat and/or local anaesthetic jelly to the nostrils; these may taste unpleasant.
- The doctor will then gently pass the bronchoscope to look inside the airways and take samples as required; you may be offered more anesthetic or sedation to help address any discomfort you may feel during the procedure.
- If necessary, the doctor may take a ‘photograph’ of any abnormalities seen within the airways.
How will I feel during the procedure?
- The procedure will not hurt you and you will be able to breathe normally during the procedure.
- It may make you cough as the bronchoscope goes into your airways.
Immediately after the procedure
- Post procedure you will be monitored for at least two hours prior to discharge.
- As your throat will have been numbed, your swallowing will not be normal and therefore it is NOT safe to eat and drink for up to two hours.
When do I know the results of the procedure?
- If samples have been taken, the results may take up to a week.
- The details of the results and necessary treatment will be discussed with you by the referring doctor.
What support will I need post procedure?
If you live on your own, you will need to arrange for someone to stay with you overnight after the procedure, however if you are unable to arrange someone to stay with you overnight after the procedure, we may have to admit you for overnight stay in the hospital. You will also need someone to drive you home.
Further Information:
If you have any further queries after the procedure please contact
Bronchoscopy coordinator
Respiratory Department
Royal Stoke University Hospital
University Hospital of North Midlands NHS Trust
Telephone number: 01782 675760
Monday to Friday 08.30 hours to 16.30 hours
Outside of these hours please contact your GP surgery for the telephone number for the emergency doctor’s service.
For further patient information please see here Bronchoscopy
What is a Liver Biopsy?
A liver biopsy involves taking a sample of liver tissue with a special needle. The sample is then examined under a microscope.
Why do I need a Liver Biopsy?
Blood tests and/or other scans may have shown a problem with your liver and it is not always possible to determine the cause or degree of these abnormalities by looking at scans alone.
A liver biopsy is the only way for your Doctor to get the information needed to make a correct diagnosis by examining a sample of liver tissue under the microscope.
Who has decided that I need the procedure?
A Consultant in charge of your care and the Interventional Radiologist (IR Doctor) performing the procedure will have assessed and discussed your case and agreed that this is the best treatment option for you.
You will have the opportunity to discuss this and can decide not to go ahead with the procedure if you wish.
Who will perform the procedure?
The procedure will be performed by a specially trained team led by a Consultant Interventional Radiologist within the Radiology Department.
Interventional Radiologists have special expertise in interpreting the images produced during the procedure and this allows them to provide you with the most appropriate treatment. These images are used to guide the needle to take the biopsy.
How do I prepare for the procedure?
The procedure is usually carried out as a day case using a local anaesthetic.
You may be asked not to eat for 4 hours before the procedure, although you may still drink clear fluids such as water up to 2 hours before the procedure. (NO MILK)
One family member or friend should accompany you to the Hospital. As there is limited space in the department, they may be asked to wait in the main X-ray reception.
Before coming into Hospital, you will have been asked about certain risk factors for vascular diseases unless you come into Hospital as an emergency. These factors include checking your blood pressure and your kidney function
Medication assessment
You will be invited for an assessment with a member of the IR Team prior to the procedure.
You will have the opportunity to discuss your procedure and any necessary changes to your medication or any blood tests needed.
The Doctor will need to see a list of all of your medications (tablets, inhalers, creams).
Please bring a copy of your current prescription with you.
If you are taking an anticoagulation drug such as Warfarin, Heparin (Dalteparin, Enoxaparin, Tinzaparin) or a direct acting oral anticoagulant (DOAC) (Apixaban, Rivaroxaban, Dobigatran), this may need to be stopped before the procedure and you may require admission to Hospital to give you alternative medication
- if you have any allergies or have previously had an allergic reaction to X-ray dye (contrast agent) or are allergic to iodine or if you think you may be pregnant, please inform the Interventional and Day Case Support Team as soon as you receive your appointment letter.
- If you are a diabetic and have an afternoon appointment for your procedure, your medication may need to be adjusted. Please therefore phone the Interventional and Day Case Support Team on receipt of your appointment letter so that they can advise you.
- Your Doctor will advise you about any changes needed to your normal medication.
Before the procedure?
- You will be greeted and asked to put on a Hospital gown.
- The IR Doctor will discuss your medications with you once again.
- You will be asked to sign a Hospital consent form agreeing to have the procedure and you will be given the opportunity to ask questions.
- A small cannula (thin tube) will be placed into a vein in your arm for access in case medication is needed.
During the procedure?
- You will be asked to lie on a trolley or a bed flat on your back or on your side.
- You will have your blood pressure, pulse , temperature and oxygen saturations recorded pre and post procedure.
- You may be given oxygen if applicable for the procedure.
- Your liver will be scanned using ultrasound to choose where the most suitable place for biopsy is. A small temporary mark will be made on your skin to mark the spot.
- The skin where the mark is located will be cleaned with antiseptic and you will be covered with sterile drapes.
- A liver biopsy is performed under sterile conditions by Interventional Radiologists and Radiology Nurses who wear sterile gloves to carry out the procedure.
- A local anaesthetic will be injected into your skin to numb the area and will sting for a short time when it is first injected.
- A small incision is made in the skin to accommodate the needle.
- The Radiologist then uses a special needle which is put in through the skin and guided with ultrasound to remove a small piece of liver tissue. Two samples may be taken.
- The sample is then sent to the laboratory for microscopic examination.
- The entry site is cleaned and a dressing applied.
- The procedure is generally pain free, however, occasionally it may hurt.
- The position in which you will be asked to lie may be uncomfortable for a short time during the biopsy.
- Tell the Nurse if you experience any pain during the procedure as pain relief can be given.
- Images may be taken during the procedure to confirm biopsy site.
- The procedure normally takes around 1 hour however, the precise duration of each procedure may vary.
What happens after the procedure?
- You will be taken back to the ward or recovery area so that you can be observed and the treatment site checked.
- Routine observations, including pulse, temperature and blood pressure will also be carried out.
- You will need to lie flat on your back or side for 2-3 hours. You will remain in bed for a total of 4-6 hours and you will be advised when you can sit up and start to move about.
- The IR Nurse will let you know when you can eat and drink after your procedure.
- If you attend as a Daycase and all your checks are normal, you should go home the same day. However you should rest for the remainder of the day
- If you are staying in Hospital as an inpatient following your biopsy, the after care is the same and your Doctors on the ward will say when you may go home.
- You will need a responsible adult to take you home by car or taxi. We do not recommend using public transport in case you feel unwell.
- You should have a responsible adult to stay with you overnight.
- Do not drive for 48 hours after the procedure, and only drive when you feel safe to do so.
- Do not go to work the day after the procedure.
- Avoid any strenuous exercise or lifting for 48 hours after the procedure.
- Keep a regular check on the biopsy site for bleeding.
- You can shower 24 hours after the procedure and bath 48 hours after procedure.
- Simple painkillers like paracetamol, might be useful for any post procedure discomfort.
- The Doctor who referred you will arrange a follow up to discuss the results
What are the risks of an Liver Biopsy?
It is a very safe procedure, however, all medical procedures involve an element of risk.
The specific risks concerning your procedure will be discussed in detail with the Doctors before you sign the consent form.
They include:
- A small bruise (Haematoma) around the site of the biopsy in the skin can occur, but this is quite normal. The bruise should not be painful and will heal.
- There is a small risk of internal bleeding after the biopsy. If there is an unexpected amount of bleeding you may need further treatment such as a blood transfusion or a special X-ray test called an Angiogram which can find where you are bleeding from and sometimes stop it.
What happens next?
Your follow up will be explained to you on discharge and you will be seen some time after your procedure by the referring Consultant Team.
You should be able to resume most normal activities within 24 hours.
Do not drive or do any strenuous activities for 48 hours following the procedure.
Seek Help using the contact details below if:
- You notice any new bleeding at your biopsy site.
- Have any pain that is not controlled by painkillers.
- Fever or flu like symptoms could indicate infection.
Contact Details
If you need help or advice, please contact the Radiology Day Case Unit Tel: 01782 679911 Monday to Friday 7.30am to 10.00pm.
Day Case Support Team Tel: 01782 679040 Monday to Friday 9.00am to 5.00pm. Outside of normal working hours, contact your GP or NHS Direct on 111.
If you need urgent attention, visit your nearest A & E department.
For further patient information please see here: Liver Biospy
Location for pleural procedures
Pleural Procedures are undertaken in the Main Building on Lower Ground 1 in the endoscopy department. Please allow 2 hours for the hospital visit.
Types of pleural procedure
Thoracic ultrasound scan: A Thoracic Ultrasound Scan is a bedside ‘jelly scan’ of the chest (similar to ultrasound scans used with pregnant women) to check if there is any abnormal fluid accumulation in the pleural cavity (between chest wall and lung) and to mark the area prior to a pleural procedure.
Pleural aspiration: A procedure involving passing a small needle, under local anaesthetic, into the pleural cavity (between chest wall and lung) to remove abnormal accumulation of fluid or air. Pleural Aspiration procedures can be for diagnostic purposes (where 20-50mls fluid is taken and sent to lab for analysis) or for therapeutic purposes (where up to a litre of fluid could be removed to help breathing).
Imaging-assisted pleural biopsy drainage
Chest drain: A small plastic tube is inserted into the pleural cavity (between chest wall and lung) to drain abnormal accumulation of fluid or air in the pleural cavity. The tube is stitched onto skin and connected to a bottle. The drain can be in place for a few days to drain all the fluid or air.
Thoracoscopy: A minimally invasive procedure that allows the doctor to look at the lining (pleura) of the lungs and rib cage. It involves inserting a thin tube with a bright light and video chip at the end through a small cut made in the side of your chest wall.
Links to leaflets and easy read.